Introduction
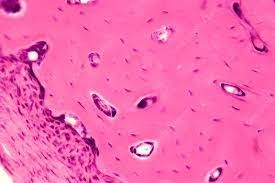
- Decalcification is a critical preparatory step in histology, particularly for hard tissues such as bone and teeth, which contain large amounts of calcium that make them challenging to section.
- Proper decalcification is essential to ensure clear microscopic examination without compromising cellular details.
- The goal is to achieve an ideal balance between adequately softening the tissue for slicing and preserving tissue structure, minimizing cell loss, and maintaining staining quality.
Biopsy
- A biopsy is a diagnostic technique that involves removing a small amount of tissue from the body to examine it under a microscope.
- It can detect cancer, infections, inflammatory or degenerative conditions, and metabolic diseases affecting bones (e.g., osteoporosis, Paget’s disease).
- In hard tissue biopsies, decalcification is crucial, as calcified tissues are too hard for thin sectioning in traditional microtomes.
- Decalcification prepares these samples for sectioning, staining, and detailed microscopic evaluation.
Factors Affecting Decalcification
- Tissue Type and Density:
- Dense tissues (e.g., cortical bone) require longer decalcification than spongy bones or other mineralized tissues.
- Age-related changes can also affect bone density and influence decalcification time.
- Sample Size:
- Larger samples take longer to decalcify. Cutting the tissue into smaller pieces can speed up the process and improve consistency.
- Concentration of Decalcifying Agent:
- Higher concentrations of decalcifying agents result in faster decalcification but can risk tissue damage, particularly affecting cellular and nuclear detail.
- Temperature:
- Higher temperatures accelerate decalcification but can damage cellular structures and reduce staining quality.
- Room temperature is generally preferred to balance time and tissue preservation.
- pH Level:
- Acidic pH favors decalcification but too low a pH can damage proteins. Chelating agents, typically neutral to slightly basic, are better at preserving tissue integrity.
- Time:
- Prolonged decalcification can lead to loss of cellular components and tissue integrity. Monitoring with end-point testing helps avoid over-decalcification.
Methods of Decalcification
- Acid Decalcification:
- Mechanism: Uses acidic solutions to dissolve calcium and magnesium salts.
- Use: Quick, suitable for time-sensitive cases.
- Consideration: Strong acids work faster but may alter cellular morphology.
- Chelation:
- Mechanism: Chelating agents, such as EDTA, bind calcium ions without altering pH significantly.
- Use: Preserves cellular and nuclear details better than acids, ideal for detailed cellular studies.
- Consideration: Very slow and may require several weeks.
- Ion Exchange:
- Mechanism: Resins exchange calcium ions with sodium or hydrogen ions in solution.
- Use: Faster than chelation and preserves tissue structure well.
- Consideration: Requires specialized resins and apparatus.
- Electrolytic Decalcification:
- Mechanism: A weak electric current accelerates the decalcification process.
- Use: Rapid for urgent biopsies but less commonly used due to specialized equipment needs.
- Consideration: Risk of heat damage if not carefully monitored.
Principle of Decalcification
- Decalcification removes calcium and magnesium salts from tissue by dissolving them into a solution.
- Acids work by ionizing calcium ions into the solution, whereas chelating agents form stable, water-soluble complexes with calcium ions.
- A careful balance in this reaction ensures that calcium salts are fully removed without affecting the tissue proteins and cellular structures needed for diagnostic purposes.
Types of Decalcifying Agents
- Strong Acids
- Examples: Nitric acid, hydrochloric acid, sulfuric acid.
- Mechanism: Dissolves calcium salts rapidly by breaking down calcium phosphate and other calcium-containing compounds.
- Advantages:
- Very fast-acting, making it suitable for urgent cases.
- Effective for dense, calcified tissue.
- Disadvantages:
- It can cause cellular distortion and loss of nuclear detail, potentially affecting staining.
- Over-decalcification is common with prolonged exposure, which can compromise tissue morphology.
- Applications: Often used in clinical settings where quick results are needed.
- Weak Acids
- Examples: Formic acid, acetic acid, picric acid.
- Mechanism: Slowly removes calcium ions without disrupting cellular structures as severely as strong acids.
- Advantages:
- Provides better preservation of cellular structure than strong acids.
- Less likely to cause tissue distortion, making it useful for studies where cellular detail is crucial.
- Disadvantages:
- Slower than strong acids, making it less suitable for urgent cases.
- It may still cause some structural degradation with extended exposure.
- Applications: Preferred for routine histopathology where preserving tissue details is essential.
- Chelating Agents
- Examples: EDTA (ethylene diamine tetra-acetic acid).
- Mechanism: Binds to calcium ions to form a stable, water-soluble complex, which is then washed away.
- Advantages:
- Superior preservation of cellular and nuclear detail, as it does not dissolve or disrupt tissue structure.
- Minimal risk of over-decalcification; pH-neutral or slightly alkaline solutions are often used to maintain tissue integrity.
- Disadvantages:
- Extremely slow; can take days to weeks, especially for dense bone tissue.
- Requires regular monitoring of pH and solution strength.
- Applications: Ideal for delicate, highly detailed histopathological studies, particularly for research or specialized medical diagnoses.
- Ion-Exchange Resins
- Examples: Ammonium ion exchange resins.
- Mechanism: Removes calcium ions from the solution, speeding up decalcification by replacing calcium with sodium or hydrogen ions.
- Advantages:
- Preserves cellular and tissue morphology relatively well.
- Faster than chelating agents but gentler than strong acids.
- Disadvantages:
- Specialized equipment and careful monitoring are required.
- Applications: Useful in labs with high sample throughput, where maintaining tissue integrity and faster processing are both important.
- Electrolytic Decalcification (less commonly used)
- Mechanism: Uses a weak electric current to accelerate calcium removal from tissues.
- Advantages:
- Rapid decalcification is useful for larger samples in a shorter time.
- Disadvantages:
- Requires careful control of temperature and electric current to prevent heat damage.
- Rarely used in standard practice due to equipment requirements and complexity.
- Applications: Limited use, mainly in specialized or experimental histology settings.
Decalcifying Fluids
1. Gooding and Stewart’s Fluid
Composition:
-
10% Formalin – 100 ml
-
Formic acid – 10 ml
Features:
-
Moderately rapid decalcifier (slower than nitric acid but faster than chelating agents).
-
Preserves tissue morphology better than nitric acid.
-
Good preservation of nuclear details.
-
Less damage to cytoplasm compared to strong acids.
-
Can be used for relatively large specimens.
Uses:
-
Routine decalcification of bone and calcified tissues.
-
Preferred where both speed and morphology preservation are important.
2. Citrate–Citric Acid Buffer
Composition:
-
20% Sodium citrate solution – 200 ml
-
40% Citric acid solution – 15 ml
-
Distilled water – to make 1000 ml
Features:
-
Very gentle decalcifier (acts as a chelating agent).
-
Excellent preservation of nuclear and cytoplasmic morphology.
-
Preserves enzymes and antigenicity → ideal for enzyme histochemistry and immunohistochemistry (IHC).
-
Decalcification speed: slowest among commonly used agents.
-
Requires frequent solution changes.
Uses:
-
Recommended for research purposes.
-
Used when IHC, special stains, or enzyme studies are required.
-
Best for delicate tissues (e.g., small bone biopsies).
3. Jenkins Fluid
Composition:
-
10% Formic acid – 100 ml
-
10% Formalin – 80 ml
-
Sodium chloride – 10 g
Features:
-
Provides a balance between speed and preservation.
-
Better nuclear staining than nitric acid.
-
Less destructive to tissues compared to strong acids.
-
Moderately fast.
-
Easy to prepare and use.
Uses:
-
General-purpose decalcifier for bone, teeth, and calcified specimens.
-
Suitable for routine diagnostic labs.
-
Good when both morphology and staining quality are important.
4. Formal Nitric Acid
Composition:
-
10% Formalin – 100 ml
-
10% Nitric acid – 10 ml
Features:
-
Very rapid decalcification (much faster than formic acid-based fluids).
-
Useful when urgent diagnosis is required.
-
Serious drawback: prolonged exposure → causes tissue damage, loss of nuclear details, poor staining.
-
Produces tissue hardening.
-
Can impair subsequent staining techniques.
Uses:
-
Emergency decalcification (e.g., urgent biopsy diagnosis).
-
Used when speed is more important than preservation.
Procedure
- Fixation:
- Fix tissue in 10% neutral buffered formalin to preserve cellular structures before decalcification.
- Washing:
- Wash the tissue in running water to remove excess formalin, preventing chemical interactions with decalcifying agents.
- Decalcification:
- Place tissue in the selected decalcifying solution. Maintain regular checks for completion using physical tests or chemical methods.
- End-Point Testing:
- Physical tests, like flexibility assessment or chemical tests, such as the ammonium oxalate test, verify calcium removal.
- Rinsing:
- Rinse thoroughly to remove any residual decalcifying agent, preventing interference with staining.
- Embedding:
- After decalcification, the tissue undergoes dehydration, clearing, and embedding in paraffin wax. Proper embedding enables thin sectioning and preserves morphological details.
Advantages and Disadvantages of Decalcifying Agents
Each decalcifying agent has specific advantages and disadvantages that make it suitable for certain tissue types, time requirements, and detail-preserving needs in histopathology.
1. Strong Acids (e.g., Nitric Acid, Hydrochloric Acid)
- Advantages:
-
- Speed: Very fast decalcification, often within hours, suitable for urgent cases where quick results are necessary.
- Effectiveness: Efficiently decalcifies dense, highly calcified tissues such as cortical bone.
- Disadvantages:
-
- Tissue Damage: High potential for cellular and nuclear damage, which may affect morphological details and staining quality.
- Risk of Over-Decalcification: Prolonged exposure can lead to loss of structural integrity, making the tissue less informative under a microscope.
2. Weak Acids (e.g., Formic Acid, Acetic Acid)
- Advantages:
-
- Better Preservation: More gentle on tissues than strong acids, leading to better cellular details and morphology preservation.
- Controlled Decalcification: Slower action reduces the risk of over-decalcification, which is useful in routine histopathology.
- Disadvantages:
-
- Slower Process: Takes longer than strong acids, which can be a drawback in time-sensitive cases.
- Limited Use for Dense Tissues: This may not be as effective on extremely dense or highly calcified tissues, requiring longer decalcification.
3. Chelating Agents (e.g., EDTA)
- Advantages:
-
- Excellent Preservation: Maintains cellular and nuclear detail, ideal for samples requiring detailed histological examination.
- No Over-Decalcification: Non-destructive process; tissue can stay in EDTA for extended periods without risking tissue damage.
- Disadvantages:
-
- Very Slow: Requires days to weeks, especially for dense tissues, which is impractical in settings requiring rapid results.
- pH Sensitivity: Needs careful pH monitoring and buffering, adding complexity to the process.
4. Ion-Exchange Resins
- Advantages:
-
- Moderate Speed: Faster than chelation but gentler than acid decalcification, balancing speed and tissue preservation.
- Good Preservation: Maintains tissue morphology reasonably well, suitable for diagnostic labs with higher sample volumes.
- Disadvantages:
-
- Equipment Requirement: Ion-exchange equipment may not be available in all labs.
- Routine Monitoring Needed: Requires careful monitoring to avoid prolonged exposure, as it may degrade tissue if left too long.
5. Electrolytic Decalcification
- Advantages:
-
- Rapid Decalcification: Provides one of the quickest decalcification methods, useful for large or thick tissue samples.
- Controlled Decalcification: This can be adjusted by regulating the electric current.
- Disadvantages:
-
- Specialized Equipment: Requires electrolytic setup, which is costly and less commonly available.
- Risk of Heat Damage: Electric current can generate heat, risking thermal damage to tissue if not carefully controlled.