Introduction
- Dermatophytes are a group of fungi that primarily infect keratinized tissues of the skin, hair, and nails, causing a variety of superficial infections known as dermatophytosis.
- These infections, commonly called tinea or ringworm, can affect humans and animals, with humans being the primary hosts.
- Dermatophytes thrive in warm, moist environments, making them particularly common in tropical climates.
- These highly contagious fungal infections can spread through direct contact with infected individuals or contaminated objects such as clothing, towels, and footwear.
- Dermatophyte infections typically present as itchy, red, and scaly patches on the skin, but they can also lead to nail and hair involvement.
Etiology
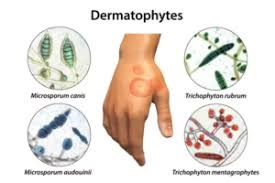
The causative agents of dermatophytosis are fungi that belong to the genera Trichophyton, Microsporum, and Epidermophyton. These fungi are keratinophilic, which can utilize keratin as a nutrient source. The most common dermatophytes include:
- Trichophyton species: These are the most common causative agents of dermatophytosis. Several species in this genus, such as Trichophyton rubrum, Trichophyton mentagrophytes, and Trichophyton tonsurans, are responsible for human infections. T. rubrum is particularly notorious for causing chronic dermatophyte infections, especially tinea pedis (athlete’s foot), tinea corporis (body ringworm), and tinea unguium (onychomycosis).
- Microsporum species: Microsporum canis is a common cause of tinea corporis and tinea capitis (scalp ringworm), often transmitted from pets, especially cats and dogs, to humans. Microsporum gypseum is another species that can infect humans, primarily through exposure to soil.
- Epidermophyton species: The genus Epidermophyton includes Epidermophyton floccosum, which is known to cause tinea cruris (jock itch) and tinea pedis.
Specimens
The type of specimen collected for diagnosing dermatophyte infections depends on the location and type of infection. Common specimens include:
- Skin Scraping: Skin scrapings from the affected area are commonly obtained for superficial infections. These samples should include infected and healthy-looking skin to ensure fungal elements are present.
- Hair Samples: In cases of tinea capitis, hair samples, including broken hair shafts or scalp scrapings, may be collected.
- Nail Clippings: For onychomycosis (nail infection), nail clippings or scrapings from the affected nails are the specimen of choice.
- Biopsy: In more severe cases or when the infection involves deeper tissues, a biopsy may be performed. The tissue sample is then examined for fungal elements.
- Swabs: Swabs can collect samples from the infected sites for moist areas like the groin or between the toes.
Direct Microscopic Examination
Direct microscopic examination is a key diagnostic tool for identifying dermatophyte infections. Common techniques used for this purpose include:
- KOH (Potassium Hydroxide) Preparation: A skin scraping, hair sample, or nail clipping is treated with KOH, which dissolves keratin, allowing the fungal elements to be more visible under the microscope. Dermatophytes can be identified as septate hyphae (branching filaments) and occasionally as arthroconidia (spores). Hair specimens often show infected hair shafts with spores attached.
- Wood’s Lamp Examination: The Wood’s lamp emits ultraviolet light, which causes certain dermatophytes, such as Microsporum canis, to fluoresce with a characteristic greenish-yellow color. This method is particularly useful for diagnosing tinea capitis.
- Gram Stain: Although not as commonly used as KOH preparation, a Gram stain can also reveal fungal elements in clinical samples. Dermatophytes appear as Gram-positive, septate hyphae or conidia.
- India Ink Staining: This method can be used in suspected fungal infections involving deeper tissues, though it is not commonly used for dermatophytes.
- Lactophenol Cotton Blue Staining: This is a fungal-specific stain used for confirming the identity of dermatophytes in culture. It stains the fungal structures, allowing them to be visible under a microscope.
Culture and Identification
Culturing dermatophytes is essential for confirming the diagnosis and identifying the species involved, which helps guide treatment decisions. The following methods are commonly used for culturing dermatophytes:
- Culture Media: Dermatophytes are typically cultured on Sabouraud dextrose agar (SDA) or Dermatophyte test media (DTM). This selective medium contains antifungal agents to inhibit the growth of bacteria and other fungi. On DTM, dermatophytes typically produce a color change in the medium (from yellow to red) due to alkaline byproducts of fungal growth.
- Incubation Conditions: Dermatophyte cultures are incubated at room temperature (25-30°C) for 1-3 weeks, growing relatively slowly. Fungal growth is observed as colonies that may be creamy, white, or yellow, and some species may have a characteristic appearance, such as the “cottony” texture of Trichophyton rubrum.
- Colony Morphology: The morphological features of the colony, such as its size, texture, color, and the presence of a red or yellow pigment, can help differentiate dermatophyte species.
- Microscopic Examination: After colony growth, a small piece of the colony is placed in lactophenol cotton blue or potassium hydroxide (KOH) preparation to examine the fungal structures. Depending on the species, dermatophytes typically produce septate hyphae, macroconidia, and microconidia.
- Biochemical and Molecular Identification: Some advanced methods, including DNA sequencing or PCR assays, can identify dermatophyte species based on genetic material. This can provide a more precise identification, especially in unclear morphological characteristics.
Other Laboratory Tests
Other laboratory tests may be used to complement the diagnosis of dermatophyte infections, particularly when culture results are unavailable or inconclusive:
- Wood’s Lamp Examination: This technique is especially useful for detecting infections caused by Microsporum canis, which exhibits fluorescence under UV light.
- Histopathology: In certain cases, skin biopsies or tissue samples may be examined histologically for the presence of fungal elements. Specialized stains such as PAS (Periodic Acid-Schiff) or GMS (Gomori’s Methenamine Silver) may enhance fungal hyphae’s visibility in tissue samples.
- Serological Tests: Although not routinely used, serological tests detecting antifungal antibodies or antigens can be useful in some cases, particularly for dermatophyte infections associated with systemic involvement.
- PCR-based Assays: PCR tests can detect the DNA of dermatophytes in clinical specimens, which is particularly useful for identifying species that are difficult to culture or when the infection is deep or chronic.
Pathogenesis
Dermatophyte infections are caused by the ability of these fungi to invade and proliferate in the keratinized tissues of the skin, hair, and nails. The pathogenesis involves several steps:
- Attachment to Keratin: Dermatophytes secrete enzymes, such as keratinases, that break down keratin, allowing the fungi to adhere to and invade the skin, hair, and nails.
- Invasion and Colonization: Once attached, dermatophytes proliferate using keratin as a nutrient source. The infection is usually confined to the stratum corneum of the skin, the hair shaft, or the nail, causing superficial inflammation.
- Immune Response: The host immune system responds to the dermatophyte infection by triggering an inflammatory response. This leads to redness, itching, and scaling in the affected areas. The immune response may result in deeper tissue involvement in more severe cases, particularly in immunocompromised individuals.
- Dissemination: In rare cases, dermatophytes can disseminate to deeper tissues, especially in individuals with weakened immune systems, such as those with diabetes, HIV/AIDS, or cancer.
Treatment of Dermatophyte Infections
The treatment of dermatophyte infections depends on the location and severity of the infection and the species of dermatophyte involved. Treatment options include:
- Topical Antifungal Agents: For localized and superficial infections, over-the-counter antifungal creams, ointments, or powders are commonly used. These may include:
- Terbinafine (Lamisil)
- Clotrimazole (Lotrimin)
- Miconazole (Micatin)
- Ketoconazole
Topical treatment is typically effective for infections like tinea corporis, tinea pedis, and tinea cruris.
- Oral Antifungal Agents: For more extensive or recalcitrant infections, oral antifungal medications may be necessary. Common oral antifungals include:
- Terbinafine
- Griseofulvin (especially for tinea capitis or onychomycosis)
- Fluconazole
- Itraconazole
Oral treatment is especially important for nail infections (onychomycosis) or widespread tinea infections.
- Nail Infections: Onychomycosis may require prolonged treatment (3-6 months) with oral antifungals like terbinafine or itraconazole.
- Hygiene and Prevention: To prevent recurrence and the spread of infection, patients should maintain good hygiene, avoid sharing personal items like towels or combs, and wear loose-fitting clothing. For athletes, changing socks frequently and using antifungal powders can help prevent tinea pedis.