Determination of Malaria Parasites
- The thick blood smear concentrates Plasmodium parasites, making them easier to detect, while the thin smear allows detailed examination of the parasite’s morphology for species identification.
- Methanol fixation preserves the integrity of cells and parasites.
- Giemsa staining enhances the visibility of parasites by differentiating them from red blood cells.
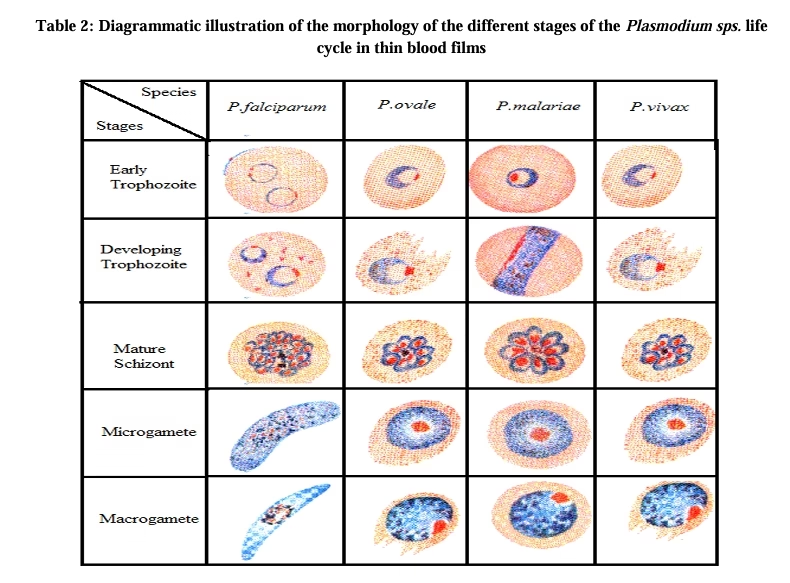
- The smears are examined under high magnification to identify parasite stages (e.g., rings, trophozoites, schizonts, gametocytes) and species.
- Microscopic examination helps detect the presence and species of Plasmodium.
- Interpretation assesses parasite load, confirming the diagnosis of malaria based on morphological features and species-specific characteristics observed in the smear.
Requirements
-
Glass Slides
- Spreader Slide
-
Lancets or Needles
-
Methanol
-
Giemsa Stain
-
Gloves
- EDTA Whole Blood
Preparation of the Blood Smears
Thick Blood Smear:
-
-
Take a drop of blood: A drop of blood is placed in the center of a clean glass slide.
-
Spread the blood: Using the edge of another slide (or a spreader slide), spread the blood in a circular motion over a larger area of the slide, covering a larger surface.
-
Leave a thicker film: The blood should form a thick, uneven film with a larger area of the smear compared to the thin smear.
-
Thin Blood Smear:
-
-
Take a drop of blood: A smaller drop of blood is placed near one edge of a clean glass slide.
-
Spread the blood: Using a spreader slide, spread the blood by placing the edge of the spreader at an angle to the slide and dragging it across the surface to create a thin, even layer.
-
Allow the smear to air dry: Ensure that the blood film is thin and uniform, then let it dry completely before fixing.
-
Fixing the Blood Smears
-
Thick Smear: The thick blood smear is not fixed immediately because the parasite is concentrated in the thicker part of the smear. It is left to air dry completely.
-
Thin Smear: The thin blood smear needs to be fixed to preserve the integrity of the cells and parasites. Fixing is done by:
-
Using Methanol: Immerse the thin smear into absolute methanol for 1-2 minutes. This process ensures that the blood cells and parasites are preserved on the slide.
-
Air Dry: After fixing, allow the slide to air dry before staining.
-
Staining the Blood Smears
-
Giemsa Staining: This is the most commonly used stain for malaria blood smears, as it provides clear differentiation of the parasite’s stages and the host blood cells.
Procedure for Giemsa Staining:
-
Prepare Giemsa Solution: Dilute Giemsa stain with buffered water to a 1:10 ratio (1 part Giemsa stain to 10 parts water) or use commercial ready-to-use Giemsa.
-
Stain the Slides:
-
Immerse the fixed slides (thin smear and thick smear) in the diluted Giemsa solution for 10–15 minutes.
-
Ensure that the slide is completely covered by the stain.
-
-
Rinse: After staining, rinse the slides gently with buffered or distilled water to remove excess stain.
-
Air Dry: Allow the slide to air dry completely before examination.
-
Other Stains:
-
Field’s Stain: Another alternative to Giemsa, which can be quicker to prepare but is less commonly used for malaria diagnosis.
-
Leishman Stain: Similar to Giemsa, but requires different preparation and may be less sensitive for detecting malaria.
Microscopic Examination
-
Thin Smear:
-
Examine under a microscope: Using an oil immersion lens (100x magnification), observe the thin smear.
-
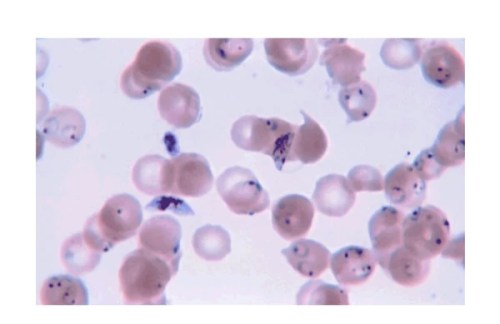
Look for parasites: Look for the malaria parasite in the red blood cells. The size, shape, and location within the red blood cell can help identify the species of Plasmodium.
-
Identify stages: Look for different stages of the parasite, including rings, trophozoites, schizonts, and gametocytes.
-
-
Thick Smear:
-
Examine the thick smear under the microscope: Start with a low power (10x) to locate areas with a high concentration of red blood cells.
-
Switch to oil immersion (100x): Examine areas with a higher concentration of red blood cells to detect the malaria parasite, which should appear as small, round forms inside or near the red blood cells.
-
Identify species: While the thick smear is helpful for detecting the presence of the parasite, the thin smear is required for species identification.
-
Interpretation of Results
-
Positive Diagnosis: If malaria parasites are seen in the blood smear, the species of Plasmodium can often be identified by the morphology and the stage of the parasite.

-
Plasmodium falciparum: Small rings, often with double chromatin dots, and the presence of crescent-shaped gametocytes.
-
Plasmodium vivax: Larger rings and trophozoites with a more prominent cytoplasm and Schüffner’s dots.
-
Plasmodium malariae: Compact rings with dark chromatin.
-
Plasmodium ovale: Similar to P. vivax, but with oval-shaped red blood cells.
-
-
Negative Diagnosis: If no parasites are seen on the smear, the diagnosis of malaria is considered negative. However, it is important to repeat the examination or use other diagnostic techniques, such as rapid diagnostic tests (RDTs) or PCR, if clinical suspicion remains high.