
AIM: Determination of Total Leukocyte Count (TLC)
Principle
- The glacial acetic acid lyses the red cells while the gentian violet slightly stains the nuclei of the leukocytes.
- The blood specimen is diluted 1:20 in a WBC pipette with the diluting fluid, and the cells are counted under low power of the microscope by using a counting chamber.
- The number of cells in undiluted blood is reported per cu mm (pl) of whole blood.

हिंदी नोट्स के लिए यहां क्लिक करें
Requirements
-
Blood Sample: EDTA blood sample
-
Dilution Fluid: Turk’s solution: A mixture of acetic acid, gentian violet (a dye), and sometimes distilled water, which also helps to enhance the visibility of WBCs.
-
Hemocytometer
-
Microscope
-
Coverslip
-
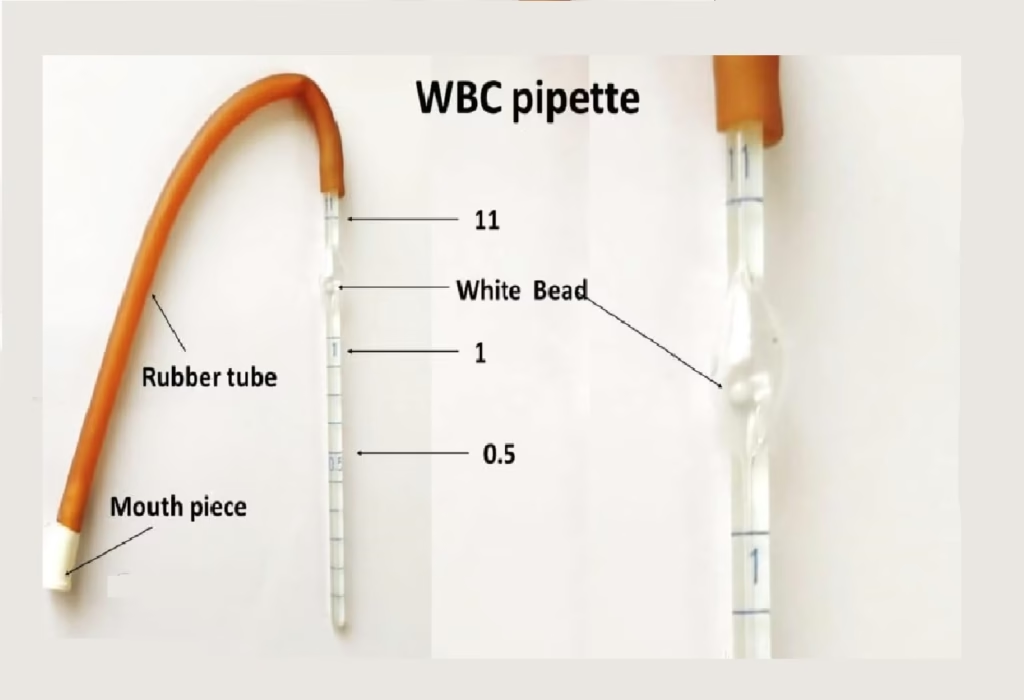
WBC Pipettes
-
Timer
Procedure
-
-
Collect a small amount of venous blood up to 0.5 marks of WBC pipette.
- Carefully wipe excess blood outside the pipette with cotton.
-
Mix the blood with a diluent (e.g., Turk’s solution) in a test tube. The typical ratio is 1 part blood to 20-100 parts of diluent, depending on the method used.
- Draw diluting fluid up to 11 mark.
-
Allow the mixture to sit for 2-5 minutes to ensure complete lysis of the red blood cells, which are removed from the sample by the solution, while the white blood cells remain intact.
-
-
Loading the Hemocytometer:
-
After the red blood cells have lysed, mix the sample gently to ensure an even suspension of white blood cells.
-
Using a pipette, carefully place a drop of the diluted sample on the hemocytometer. Avoid overloading the chamber to prevent crowding of cells.
-
Place a coverslip over the hemocytometer, ensuring the fluid spreads evenly across the grid.
-
-
Microscopic Examination:
-
Place the hemocytometer under the microscope.
-
Focus on the grid lines at 400x magnification (or higher if needed).
-
WBCs will appear as larger, round cells with a prominent nucleus compared to RBCs. They are typically colorless, though staining solutions like Turk’s solution may make them easier to distinguish.
-
-
Counting the Cells:
-
In manual counting, count the number of white blood cells in the defined area of the hemocytometer. This area typically consists of 4 large squares in the grid.
-
Each square has a specific area, and by counting the WBCs in several squares, a representative count can be obtained.
-
-
Calculation of WBC Count:
-
The WBC count is determined by counting the cells in the grid squares and applying the dilution factor. The formula is:
TLC (cells/mm³) = (Total WBC count in counted area/Area of counted grid)×Dilution Factor
-
Automated cell counters, if available, perform this calculation automatically after detecting and counting the white blood cells in the sample.
-
-
Record the Result:
-
The result is typically reported as the number of white blood cells per cubic millimeter (cells/mm³) of blood.

-

-
Clinical Significance
The total leukocyte count is an essential diagnostic tool in many clinical situations. Abnormal levels of WBCs can indicate various pathological conditions.
-
Leukocytosis (Elevated WBC Count):
-
A high TLC can be associated with:
-
Infections: Particularly bacterial infections, where the body increases WBC production to fight off pathogens.
-
Inflammation: Conditions like rheumatoid arthritis, allergies, and autoimmune disorders can cause elevated WBC counts.
-
Leukemia: A form of blood cancer that leads to the abnormal production of white blood cells.
-
Stress or trauma: Physical stressors or tissue damage can increase WBC count.
-
Drug-induced: Certain medications like corticosteroids may also lead to leukocytosis.
-
-
-
Leukopenia (Decreased WBC Count):
-
A low TLC can indicate:
-
Bone marrow disorders: Conditions like aplastic anemia or myelodysplastic syndromes can affect the production of WBCs.
-
Viral infections: Some viral infections (e.g., HIV, hepatitis) can suppress WBC production.
-
Autoimmune diseases: Conditions like lupus can cause a reduction in WBC counts.
-
Chemotherapy or radiation therapy: These treatments can lower the WBC count by affecting the bone marrow’s ability to produce new cells.
-
Nutritional deficiencies: Deficiencies in vitamin B12, folic acid, or copper can lead to low WBC counts.
-
-
-
Other Clinical Considerations:
-
Neutrophilia: A rise in neutrophils (a specific type of WBC) may occur due to bacterial infections, inflammation, or tissue damage.
-
Lymphocytosis: Increased lymphocytes can be seen in viral infections or lymphocytic leukemia.
-
Monocytosis: Elevated monocytes are often seen in chronic infections or inflammatory conditions.
-