
Introduction
-
Lipids are an important dietary component that provide energy and help in absorption of fat-soluble vitamins.
-
Due to their hydrophobic nature, lipids require bile salts and specific enzymes for digestion.
-
Most lipid digestion occurs in the small intestine with the action of pancreatic lipase.
-
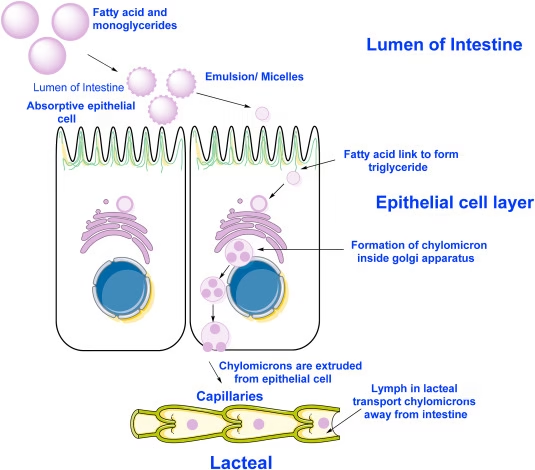
Digested lipids are absorbed as micelles and transported as chylomicrons via the lymphatic system.
-
Defects in lipid digestion or absorption lead to fat malabsorption and nutritional deficiencies.
- Digestion and absorption of lipids processes for “triglycerides, cholesterol, and phospholipids”, including specific enzymes, mechanisms, and physiological implications.
Digestion and Absorption of Triglycerides
Digestion in the Mouth:
-
Begins with lingual lipase, secreted by serous glands of the tongue.
-
Acts mainly on short- and medium-chain triglycerides.
-
The enzyme is acid-stable but exhibits minimal activity in adults.
-
Plays a significant role in infants, particularly during the digestion of milk fat.
Digestion in the Stomach: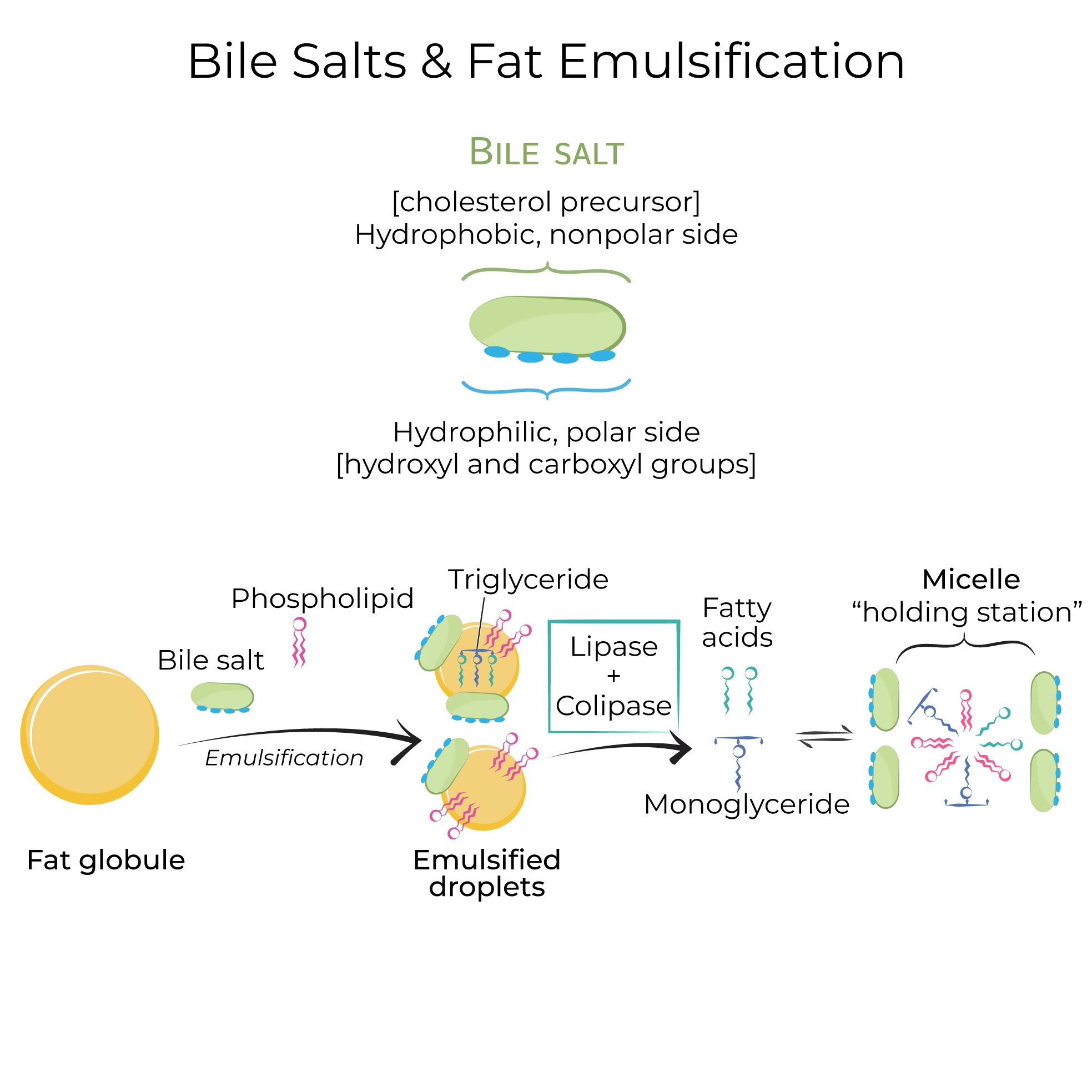
- Gastric Lipase:
- Produced by: Chief cells in the gastric mucosa.
- Function: Further hydrolyzes triglycerides into diglycerides and free fatty acids. Gastric lipase operates optimally at a low pH (around 3-6) and is particularly effective on medium-chain triglycerides.
- Mechanical Mixing:
- Churning of the stomach also helps emulsify fats, breaking them into smaller droplets, which increases the surface area for enzymatic action.
Small Intestine:
- Bile Salts:
- Produced by: Liver, stored in the gallbladder.
- Function: Upon release into the duodenum, bile salts emulsify large fat globules into smaller micelles. This process is crucial because it allows pancreatic lipase access to triglycerides.
- Pancreatic Lipase:
- Produced by: Pancreas.
- Function: Hydrolyzes triglycerides into monoglycerides and two free fatty acids. This enzyme is highly efficient and requires the presence of bile salts for optimal activity.
- Colipase:
- Produced by the pancreas (as a proenzyme, activated in the intestine).
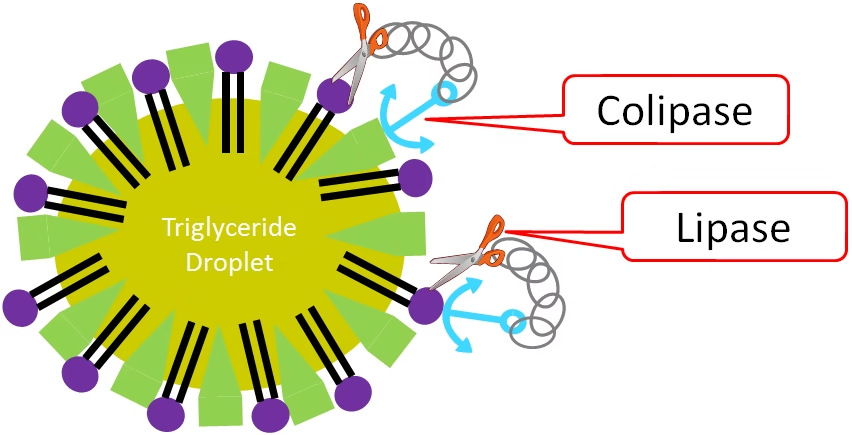
- Function: Binds to the lipid-water interface, displacing bile salts and anchoring pancreatic lipase, enhancing its ability to digest triglycerides.
- Produced by the pancreas (as a proenzyme, activated in the intestine).
Absorption: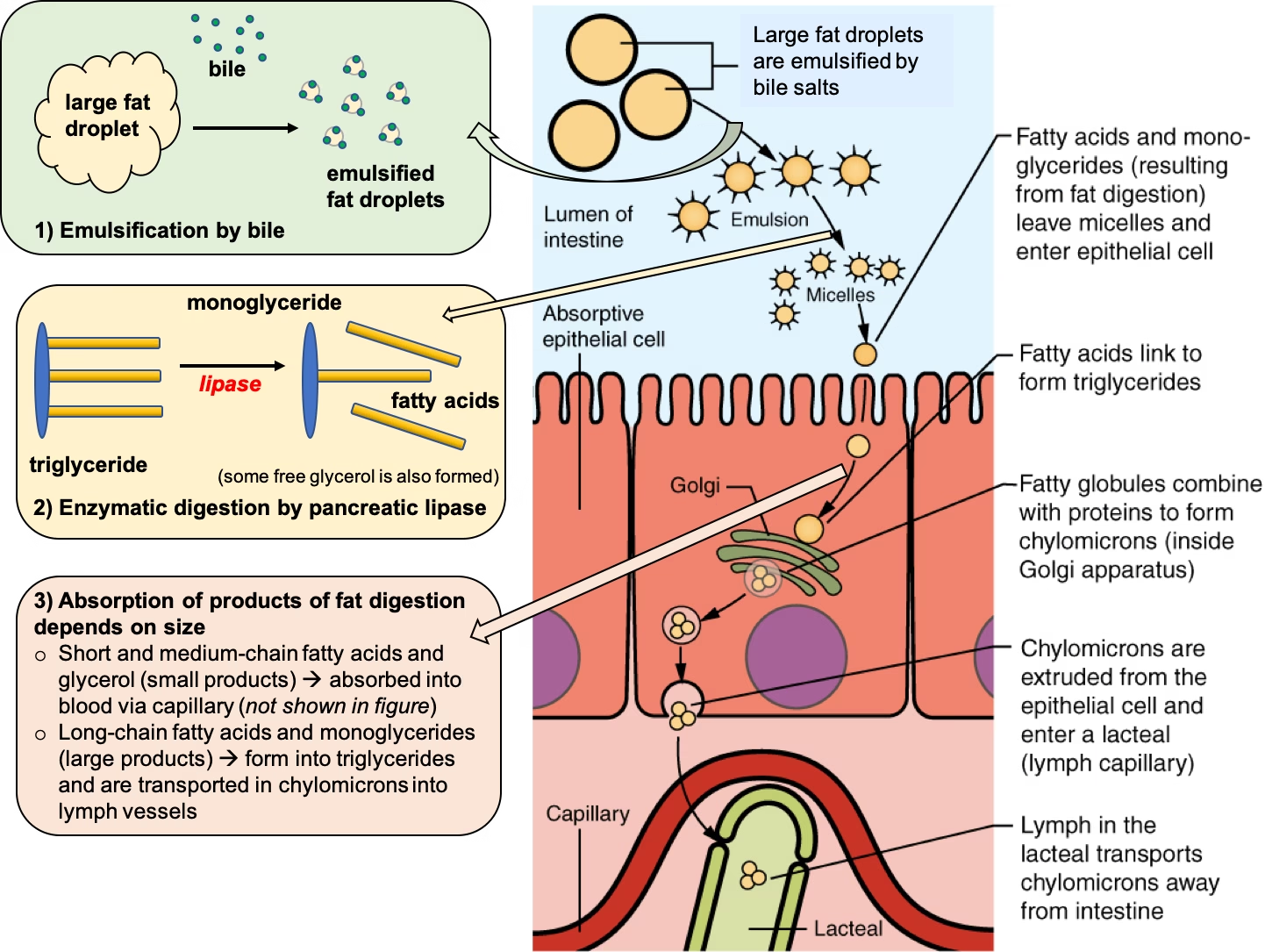
- Formation of Micelles:
- Digestion products (monoglycerides and free fatty acids) aggregate with bile salts to form micelles, transporting lipids to the enterocytes’ brush border.
- Transport into Enterocytes:
- Mechanisms:
- Passive Diffusion: Monoglycerides and free fatty acids enter enterocytes by simple diffusion due to their lipophilic nature.
- Transport Proteins: Some fatty acids may also be transported via specific fatty acid transport proteins (FAT/CD36).
- Inside Enterocytes:
- Re-esterification: Once inside, monoglycerides and free fatty acids are re-esterified into triglycerides in the smooth endoplasmic reticulum.
- Packaging into Chylomicrons: Triglycerides, along with cholesterol and phospholipids, are packaged into chylomicrons, which are large lipoprotein particles.
- Mechanisms:
Digestion and Absorption of Cholesterol
Small Intestine:
- Cholesterol Esterase:
- Produced by: Pancreas.
- Function: Hydrolyzes cholesterol esters into free fatty acids, making cholesterol available for absorption.
- Bile Salts:
- Aid in emulsifying dietary cholesterol, improving its solubility and absorption.
Absorption: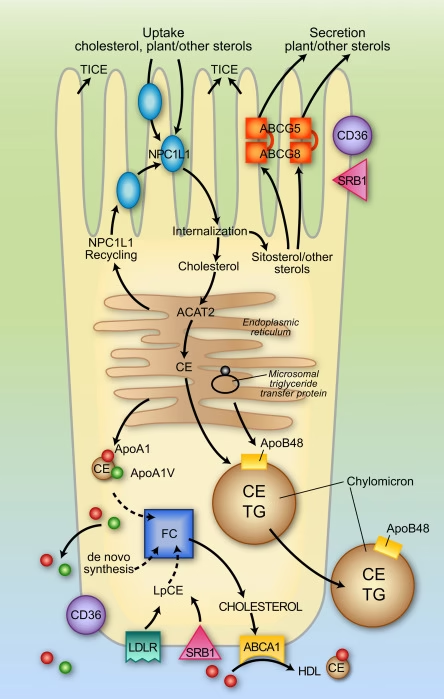
- Mechanism:
- Free cholesterol is absorbed primarily via the Niemann-Pick C1-like 1 (NPC1L1) transporter, facilitating its uptake into enterocytes.
- Some cholesterol is also absorbed through passive diffusion.
- Inside Enterocytes:
- Re-esterification: Free cholesterol can be re-esterified into cholesterol esters for storage or incorporation into chylomicrons.
Digestion and Absorption of Phospholipids
Small Intestine: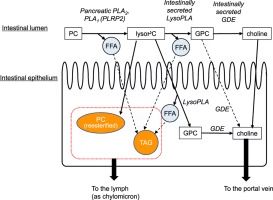
- Phospholipase A2:
- Produced by: Pancreas.
- Function: Hydrolyzes phospholipids (e.g., lecithin) into lysophospholipids and free fatty acids. This step is crucial for releasing fatty acids from phospholipid molecules.
Absorption:
- Mechanism:
- Lysophospholipids can be absorbed via passive diffusion or specific transporters, similar to free fatty acids.
- Inside Enterocytes:
- Lysophospholipids can be reassembled into phospholipids or incorporated into chylomicrons.
Disorders
Abnormalities in lipid digestion and absorption can lead to various health issues. Here are some common conditions and their underlying mechanisms:
Malabsorption Syndromes
These conditions hinder the body’s ability to absorb lipids effectively.
- Celiac Disease:
- Mechanism: An autoimmune disorder that damages the small intestine’s lining in response to gluten, impairing nutrient absorption, including lipids.
- Symptoms: Diarrhea, weight loss, bloating, and nutrient deficiencies.
- Chronic Pancreatitis:
- Mechanism: Inflammation of the pancreas reduces the secretion of digestive enzymes, including pancreatic lipase, leading to poor digestion of fats.
- Symptoms: Steatorrhea (fatty stools), abdominal pain, weight loss, and nutrient deficiencies.
- Short Bowel Syndrome:
- Mechanism: A condition resulting from surgical removal of part of the small intestine, leading to reduced absorption surface area.
- Symptoms: Diarrhea, dehydration, and malnutrition due to inadequate absorption.
Lipid Metabolism Disorders
These genetic disorders affect lipid processing and transport.
- Familial Hypercholesterolemia:
- Mechanism: Genetic mutations affect the LDL receptor, leading to elevated levels of low-density lipoprotein (LDL) cholesterol in the blood.
- Symptoms: Early onset of cardiovascular disease and cholesterol deposits (xanthomas).
- Lipid Storage Diseases:
- Examples: Tay-Sachs disease and Gaucher’s disease.
- Mechanism: Enzyme deficiencies lead to the accumulation of lipids in tissues.
- Symptoms: Vary widely but can include neurological symptoms and organomegaly.
Bile Acid Deficiency
Bile acids are essential for lipid emulsification and absorption.
- Biliary Atresia:
- Mechanism: A congenital condition where bile ducts are absent or damaged, preventing bile from reaching the intestine.
- Symptoms: Jaundice, poor weight gain, and fat malabsorption.
- Cholecystectomy:
- Mechanism: Surgical removal of the gallbladder can lead to reduced bile storage, affecting lipid digestion, especially after high-fat meals.
- Symptoms: Diarrhea and steatorrhea.
Intestinal Disorders
Conditions that affect the integrity of the intestinal lining can impair absorption.
- Irritable Bowel Syndrome (IBS):
- Mechanism: A functional gastrointestinal disorder that may affect the absorption of nutrients, including lipids, due to altered gut motility.
- Symptoms: Abdominal pain, bloating, diarrhoea, or constipation.
- Inflammatory Bowel Disease (IBD):
- Examples: Crohn’s disease and ulcerative colitis.
- Mechanism: Inflammation of the gastrointestinal tract leads to compromised absorption.
- Symptoms: Abdominal pain, diarrhoea, weight loss, and fatigue.
Excessive Fat Intake
High-fat diets can lead to various metabolic issues.
- Obesity:
- Mechanism: Excessive caloric intake, especially from fats, leads to increased adiposity and related health complications.
- Symptoms: Increased risk of diabetes, cardiovascular disease, and metabolic syndrome.
- Hyperlipidemia:
- Mechanism: Elevated levels of lipids (triglycerides and cholesterol) in the blood can result from poor dietary habits, genetic factors, or metabolic disorders.
- Symptoms: Often asymptomatic, but can lead to cardiovascular issues.
MCQs
1. Major dietary lipid is:
A. Cholesterol
B. Phospholipids
C. Triglycerides
D. Fat-soluble vitamins
2. Caloric value of lipids per gram is:
A. 4 kcal
B. 7 kcal
C. 9 kcal
D. 12 kcal
3. Initial digestion of lipids begins in the:
A. Stomach
B. Small intestine
C. Mouth
D. Colon
4. Lingual lipase is most important in:
A. Adults
B. Elderly
C. Infants
D. Adolescents
5. Gastric lipase is secreted by:
A. Parietal cells
B. Chief cells
C. Goblet cells
D. Enterocytes
6. Major site of lipid digestion is:
A. Stomach
B. Duodenum
C. Ileum
D. Colon
7. Emulsification of fats is carried out by:
A. Pancreatic lipase
B. Colipase
C. Bile salts
D. Cholesterol esterase
8. Bile salts are produced in the:
A. Gall bladder
B. Pancreas
C. Liver
D. Intestine
9. Pancreatic lipase digests triglycerides into:
A. Glycerol + fatty acids
B. 2-monoacylglycerol + fatty acids
C. Diacylglycerol only
D. Free glycerol only
10. Colipase is required for the action of:
A. Gastric lipase
B. Lingual lipase
C. Pancreatic lipase
D. Phospholipase
11. Colipase is activated by:
A. Pepsin
B. Trypsin
C. Lipase
D. Amylase
12. Phospholipids are digested by:
A. Lipoprotein lipase
B. Phospholipase A₂
C. Cholesterol esterase
D. Pancreatic amylase
13. Cholesterol esters are hydrolyzed by:
A. Lipase
B. Colipase
C. Cholesterol esterase
D. Phospholipase
14. End products of phospholipid digestion are:
A. Glycerol + fatty acids
B. Lysophospholipids + fatty acids
C. Cholesterol only
D. Triglycerides
15. Micelles are formed with the help of:
A. Lipase
B. Bile salts
C. Colipase
D. Proteins
16. Micelles transport lipids to:
A. Blood
B. Liver
C. Brush border of enterocytes
D. Colon
17. Main site of lipid absorption is:
A. Duodenum
B. Jejunum
C. Ileum
D. Colon
18. Lipids enter enterocytes mainly by:
A. Active transport
B. Facilitated diffusion
C. Passive diffusion
D. Endocytosis
19. Fatty acid transport protein is:
A. GLUT-4
B. NPC1L1
C. FAT/CD36
D. LDL receptor
20. Short-chain fatty acids are absorbed into:
A. Lymph
B. Portal blood
C. Chylomicrons
D. Bile
21. Re-esterification of lipids occurs in:
A. Mitochondria
B. Rough ER
C. Smooth ER
D. Golgi apparatus
22. Triglycerides are packaged into:
A. VLDL
B. LDL
C. HDL
D. Chylomicrons
23. Apoprotein present in chylomicrons is:
A. Apo-A
B. Apo-B48
C. Apo-C
D. Apo-E
24. Chylomicrons enter circulation via:
A. Portal vein
B. Hepatic vein
C. Lymphatic system
D. Renal vein
25. Lacteals are found in:
A. Liver
B. Pancreas
C. Intestinal villi
D. Spleen
26. Fat-soluble vitamins include:
A. B and C
B. C and K
C. A, D, E, K
D. B12 only
27. Steatorrhea means:
A. Blood in stool
B. Excess fat in stool
C. Mucus in stool
D. Water loss
28. Common cause of steatorrhea is:
A. Iron deficiency
B. Pancreatic insufficiency
C. Anemia
D. Hypertension
29. Bile salt deficiency leads to:
A. Protein malabsorption
B. Carbohydrate intolerance
C. Fat malabsorption
D. Mineral toxicity
30. Disease associated with fat malabsorption:
A. Diabetes mellitus
B. Celiac disease
C. Hypertension
D. Asthma
31. Vitamin K deficiency causes:
A. Night blindness
B. Bone pain
C. Bleeding tendency
D. Neuropathy
32. Vitamin D deficiency leads to:
A. Scurvy
B. Rickets/Osteomalacia
C. Anemia
D. Beriberi
33. Vitamin A deficiency causes:
A. Bleeding
B. Night blindness
C. Bone pain
D. Muscle weakness
34. Cholesterol absorption transporter is:
A. FAT/CD36
B. GLUT-2
C. NPC1L1
D. ABC transporter
35. Cholesterol is esterified inside enterocytes by:
A. LCAT
B. HMG-CoA reductase
C. ACAT
D. Lipase
36. Bile salts are reabsorbed in:
A. Jejunum
B. Duodenum
C. Ileum
D. Colon
37. Enterohepatic circulation refers to:
A. Lipid transport
B. Bile salt recycling
C. Protein digestion
D. Glucose metabolism
38. Pancreatic lipase works best at:
A. Acidic pH
B. Neutral pH
C. Alkaline pH
D. Very low pH
39. Gastric lipase acts best at:
A. Neutral pH
B. Acidic pH
C. Alkaline pH
D. High temperature
40. Which is NOT a function of bile salts?
A. Emulsification
B. Micelle formation
C. Enzyme digestion
D. Vitamin absorption
41. Main form of cholesterol absorbed is:
A. Cholesterol ester
B. Free cholesterol
C. HDL
D. LDL
42. Major lipid transported by chylomicrons:
A. Cholesterol
B. Phospholipids
C. Triglycerides
D. Fat-soluble vitamins
43. Absorption of lipids requires:
A. Water solubility
B. Bile salts
C. Insulin
D. Glucagon
44. Which enzyme is activated by trypsin?
A. Lipase
B. Procolipase
C. Amylase
D. Maltase
45. Lysophospholipids are absorbed by:
A. Active transport
B. Passive diffusion
C. Endocytosis
D. Pinocytosis
46. Lipid digestion products are insoluble in:
A. Fat
B. Oil
C. Water
D. Bile
47. Smooth ER is involved in:
A. Protein synthesis
B. Lipid re-esterification
C. DNA replication
D. Enzyme secretion
48. Major complication of lipid malabsorption:
A. Obesity
B. Vitamin deficiency
C. Hyperglycemia
D. Hypertension
49. Fat absorption is impaired in:
A. Obstructive jaundice
B. Iron deficiency anemia
C. Leukemia
D. Polycythemia
50. Final transport form of dietary lipids is:
A. Micelles
B. Fat droplets
C. Chylomicrons
D. Free fatty acids
Answer Key
-
C
-
C
-
C
-
C
-
B
-
B
-
C
-
C
-
B
-
C
-
B
-
B
-
C
-
B
-
B
-
C
-
B
-
C
-
C
-
B
-
C
-
D
-
B
-
C
-
C
-
C
-
B
-
B
-
C
-
B
-
C
-
B
-
B
-
C
-
C
-
C
-
B
-
C
-
B
-
C
-
B
-
C
-
B
-
B
-
B
-
C
-
B
-
B
-
A
-
C