Epithelial cells are specialised cells that form the epithelium, a continuous layer that covers body surfaces, lines cavities, and organs and constitutes glandular tissue. They are characterised by closely packed cells with minimal extracellular matrix.
General Features of Epithelial Cells
- Cellularity: Epithelial tissues are composed almost entirely of cells, with very little extracellular matrix. Cells are tightly packed, providing a barrier.
- Polarity: Epithelial cells exhibit polarity, meaning they have distinct structural and functional regions:
- Apical Surface: The uppermost layer exposed to the body’s exterior or an internal cavity. This surface may have microvilli or cilia.
- Basolateral Surface: The surface attached to the underlying connective tissue, often anchored by a basement membrane.
- Avascularity: Epithelial tissues do not contain blood vessels. They receive nutrients and oxygen through diffusion from underlying connective tissues.
- Regeneration: Epithelial cells have a high regenerative capacity, allowing them to quickly replace damaged or lost cells.
- Basement Membrane: Epithelial cells rest on a thin extracellular matrix called the basement membrane, which provides structural support and anchorage.
Functions of Epithelial Cells
- Protection: Epithelia is a barrier to protect underlying tissues from mechanical injury, pathogens, and chemical exposure (e.g., skin epithelium).
- Absorption: Epithelial cells in the intestines absorb nutrients and water (e.g., simple columnar epithelium with microvilli).
- Secretion: Glandular epithelium produces and secretes substances such as enzymes, hormones, mucus, and sweat.
- Excretion: Certain epithelial cells, such as those in the kidneys, are involved in the excretion of waste products.
- Filtration: Epithelial cells in the kidneys also filter blood.
- Sensation: Specialized epithelial cells can have sensory functions, such as taste buds in the tongue or olfactory epithelium in the nasal cavity.
Classification by Cell Shape
-
Squamous Epithelium
- Simple Squamous Epithelium:
- Structure: Composed of a single layer of flat cells.
- Function: Facilitates diffusion, filtration, and osmosis due to its thinness.
- Locations:
- Alveoli: Sites of gas exchange in the lungs.
- Endothelium: Lining of blood vessels, providing a smooth surface to reduce friction.
- Mesothelium: Lining of body cavities (e.g., pleura, peritoneum).
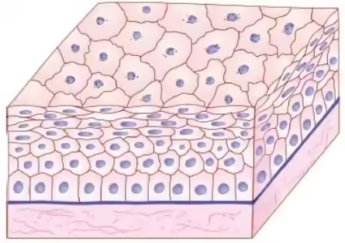
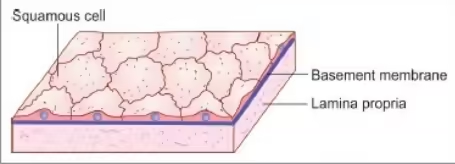
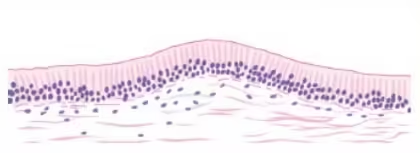
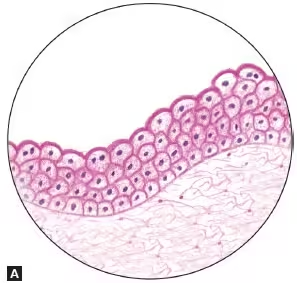
- Stratified Squamous Epithelium:
- Structure: Multiple layers of cells, with the outermost layer flat. It can be keratinized or non-keratinized.
- Function: Protects against abrasion, pathogens, and chemical exposure.
- Types:
- Keratinized Stratified Squamous Epithelium:
- Structure: Outer layers contain keratin, a protective protein.
- Location: Epidermis of the skin.
- Non-Keratinized Stratified Squamous Epithelium:
- Structure: Remains moist and lacks a keratin layer.
- Locations: Lining of the mouth, esophagus, vagina, and anal canal.
- Keratinized Stratified Squamous Epithelium:
- Simple Squamous Epithelium:
-
Cuboidal Epithelium
- Simple Cuboidal Epithelium:
- Structure: A single layer of cube-shaped cells with centrally located nuclei.
- Function: Involved in secretion and absorption due to the presence of organelles such as mitochondria and rough endoplasmic reticulum.
- Locations:
- Kidney Tubules: Facilitates reabsorption of water and solutes.
- Glands: Such as the thyroid, where hormones are produced and secreted.
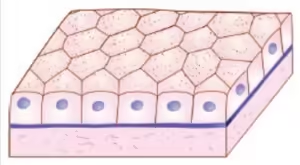
- Stratified Cuboidal Epithelium:
- Structure: Typically consists of two or more layers of cuboidal cells.
- Function: Provides protection and limited secretion.
- Locations: Found in some ducts of sweat glands, mammary glands, and salivary glands.
- Simple Cuboidal Epithelium:
-
Columnar Epithelium
- Simple Columnar Epithelium:
- Structure: A single layer of tall, column-like cells; nuclei are usually located near the base. It can have microvilli or cilia on the apical surface.
- Function: Specializes in absorption and secretion of mucus and enzymes.
- Locations:
- Digestive Tract: Lining of the stomach and intestines (with microvilli for absorption).
- Uterine Tubes: The ciliated type helps move the egg towards the uterus.
- Pseudostratified Columnar Epithelium:
- Structure: Appears stratified due to varying cell heights but is a single layer, often ciliated.
- Function: Primarily involved in the secretion and movement of mucus.
- Locations: Lining of the trachea and upper respiratory tract, where it traps particles and moves them out of the airways.
- Stratified Columnar Epithelium:
- Structure: Consists of multiple layers, with the surface layer being columnar.
- Function: Provides protection and limited secretion.
- Locations: Rare, found in some areas like the male urethra and certain ducts of glands.
- Simple Columnar Epithelium:
Classification by Number of Cell Layers
-
Simple Epithelium
Definition: Composed of a single layer of cells. Simple epithelium allows for easy diffusion, absorption, and secretion due to its thinness.
- Types:
- Simple Squamous Epithelium:
- Structure: A single layer of flat, scale-like cells.
- Function: Facilitates diffusion and filtration.
- Locations: Alveoli of lungs, lining of blood vessels (endothelium), and serous membranes (mesothelium).
- Simple Cuboidal Epithelium:
- Structure: A single layer of cube-shaped cells with centrally located nuclei.
- Function: Involved in secretion and absorption.
- Locations: Kidney tubules, ducts of small glands, and the thyroid gland.
- Simple Columnar Epithelium:
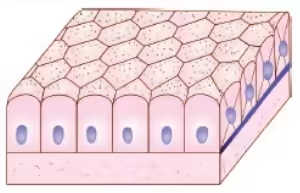
- Structure: A single layer of tall, column-like cells, often with microvilli or cilia.
- Function: Specializes in absorption and secretion of mucus and enzymes.
- Locations: Lining of the gastrointestinal tract (stomach and intestines) and the respiratory tract (with cilia in the uterine tubes).
- Pseudostratified Columnar Epithelium:
- Structure: Appears to be stratified due to varying cell heights, but is a single layer with all cells attached to the basement membrane.
- Function: Primarily involved in the secretion and movement of mucus.
- Locations: Lining of the trachea and upper respiratory tract.
- Simple Squamous Epithelium:
2. Stratified Epithelium
Definition: Composed of two or more layers of cells. Stratified epithelium provides increased protection against abrasion, pathogens, and chemical exposure.
- Types:
- Stratified Squamous Epithelium:
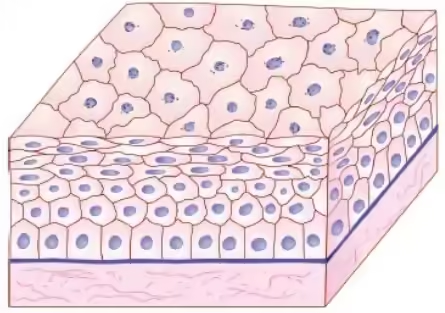
- Structure: Multiple layers of cells, with the outermost layer being flat. Can be keratinized or non-keratinized.
- Function: Protects underlying tissues from abrasion and infection.
- Types:
- Keratinized: Contains keratin, providing a tough protective layer (e.g., epidermis of skin).
- Non-Keratinized: Remains moist and is found in areas subject to abrasion (e.g., the lining of the mouth, esophagus, and vagina).
- Stratified Cuboidal Epithelium:
- Structure: Typically consists of two or more layers of cuboidal cells.
- Function: Provides protection and limited secretion.
- Locations: Found in some larger ducts of sweat, mammary, and salivary glands.
- Stratified Columnar Epithelium:
- Structure: Consists of multiple layers, with the surface layer being columnar.
- Function: Provides protection and secretion.
- Locations: Rare; found in some areas like the male urethra and certain ducts of glands.
- Stratified Squamous Epithelium:
3. Transitional Epithelium
Definition: A specialized stratified epithelium that can stretch and change shape.
- Structure: Composed of multiple layers of cells that can appear cuboidal when relaxed and squamous when stretched.
- Function: Allows for expansion and contraction, accommodating fluctuating volumes of liquid without losing integrity.
-
Location: Primarily found in the urinary bladder, ureters, and parts of the urethra. It protects against urine and allows the bladder to expand as it fills.
- Types:
Histological Features
Epithelial tissues can be examined using various histological techniques, allowing for detailed observations of their structure and function:
- Staining Techniques:
- Hematoxylin and Eosin (H&E): Commonly used for visualizing general tissue architecture. Hematoxylin stains nuclei blue, while eosin stains the cytoplasm pink.
- Periodic Acid-Schiff (PAS): Stains carbohydrates and is useful for identifying mucus-secreting cells and glycogen.
- Microscopy:
- Light Microscopy: Provides a general overview of epithelial structure and organization.
- Electron Microscopy: Offers detailed views of cell organelles, junctions, and surface modifications such as microvilli and cilia.
Applied Histology of Epithelial Cells
- Histological Techniques:
- Staining: Various techniques (e.g., H&E, PAS) help visualize epithelial cells and their organization under a microscope.
- Microscopy: Light and electron microscopy are used to examine the ultrastructure of epithelial cells and their specialized features.
- Clinical Relevance:
- Pathology: Changes in epithelial cell structure and function can indicate disease. For example, dysplasia (abnormal cell growth) can precede cancer.
- Biopsy Analysis: Histological examination of epithelial tissues from biopsies helps diagnose conditions such as tumors, infections, and inflammatory diseases.
- Immunohistochemistry: This technique can identify specific proteins expressed in epithelial cells, aiding in diagnosing certain cancers and conditions.
- Tissue Engineering: Epithelial cells are crucial in tissue engineering and regenerative medicine, particularly in developing skin grafts or repairing mucosal surfaces.