Introduction
- Fibrinogen is a soluble plasma glycoprotein produced primarily by the liver.
- It is an essential component of the coagulation cascade. It plays a critical role in hemostasis (the cessation of bleeding) by serving as the precursor to fibrin, the structural protein that forms the framework of blood clots.
- Fibrinogen is also involved in wound healing, inflammation, and cell migration.
Structure of Fibrinogen
Fibrinogen is a 340 kDa glycoprotein composed of three pairs of polypeptide chains:
- Aα (alpha), Bβ (beta), and γ (gamma).
These chains are linked together by disulfide bonds and organized into a dimeric structure.
- Central E Domain:
- Contains the thrombin cleavage sites.
- Plays a role in fibrin polymerization.
- D Domains (at the ends):
- Contain binding sites for platelets and factor XIIIa.
Synthesis of Fibrinogen
- Fibrinogen is synthesized in the hepatocytes of the liver.
- Once synthesized, it is secreted into the bloodstream, where it circulates at a concentration of approximately 200–400 mg/dL.
Physiological Role of Fibrinogen
- Coagulation:
- Fibrinogen is converted to fibrin by thrombin during the coagulation process.
- Fibrin monomers polymerize to form a fibrin clot, stabilized by factor XIIIa.
- Platelet Aggregation:
- Fibrinogen acts as a bridge between activated platelets by binding to the glycoprotein IIb/IIIa (GPIIb/IIIa) receptors on platelet surfaces.
- This promotes platelet aggregation and strengthens the initial platelet plug.
- Wound Healing and Tissue Repair:
- Fibrinogen and its degradation products facilitate cell adhesion, migration, and angiogenesis, promoting tissue repair.
- Inflammatory Response:
- Acts as an acute-phase reactant, and its levels increase during systemic inflammation.
Clinical Significance
- Normal Plasma Fibrinogen Levels: 200–400 mg/dL.
- Elevated levels: Associated with inflammation, cardiovascular disease, or pregnancy.
- Reduced levels: Seen in conditions like liver disease, disseminated intravascular coagulation (DIC), or congenital fibrinogen disorders.
Disorders Related to Fibrinogen
- Hypofibrinogenemia:
- Reduced fibrinogen levels due to liver disease, DIC, or inherited deficiencies.
- Hyperfibrinogenemia:
- Elevated fibrinogen levels are seen in inflammatory conditions, infections, or malignancies.
- Dysfibrinogenemia:
- Qualitative defects in fibrinogen function due to genetic mutations.
Mechanism of Fibrinolysis
Fibrinolysis is the process by which fibrin clots, the final coagulation product, are broken down. This process is essential for maintaining vascular integrity, preventing the persistence of blood clots, and restoring blood flow after hemostasis has been achieved.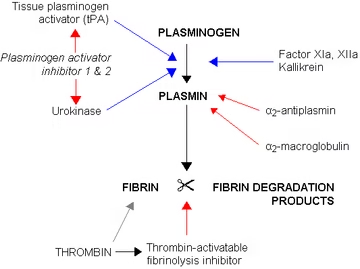
Components of Fibrinolysis
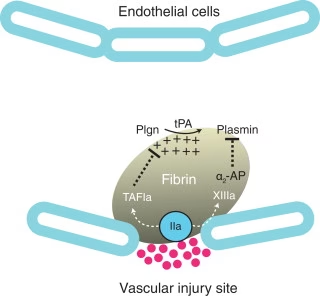
- Plasminogen:
- A glycoprotein is synthesized in the liver and circulates as an inactive zymogen.
- Incorporated into the forming clot by binding to fibrin.
- Plasmin:
- The active form of plasminogen, responsible for fibrin degradation.
- Plasmin cleaves fibrin into fibrin degradation products (FDPs) such as D-dimers, which are markers of fibrinolytic activity.
- Tissue Plasminogen Activator (tPA):
- A serine protease secreted by endothelial cells.
- Catalyzes the conversion of plasminogen to plasmin by binding to fibrin within the clot.
- Urokinase-Type Plasminogen Activator (uPA):
- Produced by endothelial cells and other tissues.
- Activates plasminogen in the fluid phase (important in tissues and extracellular matrix remodeling).
- Fibrin:
- The structural scaffold of the blood clot formed during coagulation.
- Inhibitors:
- Plasminogen Activator Inhibitor-1 (PAI-1): Regulates tPA and uPA, preventing unnecessary activation of plasminogen.
- α2-Antiplasmin: Directly inhibits free plasmin in the circulation, limiting fibrinolysis to the clot site.
Steps in the Fibrinolytic Pathway
- Plasminogen Activation:
- Plasminogen is recruited to the clot via its binding to fibrin.
- Tissue plasminogen activator (tPA) and urokinase (uPA) convert plasminogen into its active form, plasmin.
- Action of Plasmin:
- Plasmin degrades fibrin into soluble fibrin degradation products (FDPs), including D-dimers.
- Cleavage of fibrin weakens and eventually dissolves the clot.
- Regulation of Fibrinolysis:
- Tight control is required to prevent premature or excessive clot dissolution, which can lead to bleeding.
- PAI-1 inhibits tPA/uPA activity to regulate plasmin production.
- α2-Antiplasmin neutralizes free plasmin, ensuring fibrinolysis is restricted to the clot site.
- Fibrin Degradation Products (FDPs):
- The breakdown of fibrin produces FDPs, including D-dimers, which are markers of active fibrinolysis.
- Clearance:
- FDPs and D-dimers are cleared from circulation by the liver and kidneys.
Clinical Relevance of Fibrinolysis
- Hypofibrinolysis (reduced fibrinolysis): Can lead to thrombosis and clot persistence, causing conditions like stroke, myocardial infarction, or deep vein thrombosis.
- Hyperfibrinolysis (excessive fibrinolysis): Can cause bleeding disorders, as seen in disseminated intravascular coagulation (DIC), trauma, or liver disease.
Tests for Fibrinolysis
Several tests are used to evaluate the fibrinolytic system. These tests help diagnose disorders involving hyperfibrinolysis, hypofibrinolysis, or thrombotic conditions.
D-Dimer Test
- Measures the presence of D-dimers, which are fibrin-specific degradation products formed during fibrinolysis.
- Methodology:
- Immunoassays (e.g., ELISA, latex agglutination).
- Interpretation:
- High levels: Suggest active fibrinolysis, such as in DIC, pulmonary embolism, or deep vein thrombosis.
- Low levels: Absence of active fibrinolysis.
- Clinical Significance: Frequently used to exclude thromboembolic disorders.
Euglobulin Clot Lysis Time (ECLT)
- A functional test that measures the time taken for a clot to dissolve.
- Procedure:
- Euglobulin proteins (including fibrinolytic factors) are precipitated from plasma using acid.
- The proteins are redissolved, and a clot is formed using thrombin.
- The time for clot dissolution is recorded.
- Interpretation:
- Shortened lysis time: Hyperfibrinolysis (e.g., DIC, trauma).
- Prolonged lysis time: Hypofibrinolysis (e.g., liver disease, plasminogen deficiency).
Fibrin Degradation Products (FDPs) Assay
- Detects fragments of degraded fibrin or fibrinogen, indicating fibrinolytic activity.
- Interpretation:
- Elevated FDPs: Seen in DIC, hyperfibrinolysis, or excessive clot breakdown.
Plasminogen Assay
- Measures the concentration and functional activity of plasminogen in plasma.
- Clinical Use:
- Decreased levels Suggest congenital plasminogen deficiency or liver disease.
Tissue Plasminogen Activator (tPA) Activity Test
- Quantifies the activity or levels of tPA in plasma.
- Clinical Relevance:
- Elevated tPA levels: Seen in DIC or systemic inflammation.
- Low tPA levels: Suggest hypofibrinolysis.
α2-Antiplasmin Activity Test
- Measures the inhibitory capacity of α2-antiplasmin against plasmin.
- Interpretation:
- Decreased levels: Indicate excessive fibrinolysis or congenital deficiency.
Thromboelastography (TEG)
- A comprehensive test that evaluates the dynamics of clot formation, stabilization, and breakdown in real-time.
- Parameters Assessed:
- Clot strength.
- Clot lysis time.
- Clinical Use:
- Identifies fibrinolytic abnormalities in trauma, surgery, or liver disease.