Introduction
- The Hemadsorption Assay (HAD) is a fundamental virological method used to detect viruses that express hemagglutinins (HA) on the surface of infected cells.
- Some viruses, such as Influenza, Parainfluenza, Mumps, and Measles, possess HA glycoproteins that mediate red blood cell (RBC) binding.
- This unique property forms the basis of the HAD assay, making it a valuable tool for virus identification and research.
- The HAD assay is particularly useful for detecting viruses that do not cause visible cytopathic effects (CPE) in cell cultures.
- Since hemadsorption occurs even without significant cellular damage, it provides an alternative means of virus detection.
- The test is simple, cost-effective, and widely used in clinical and research laboratories to confirm viral infections.
Principle
The principle of the Hemadsorption Assay is based on the expression of viral hemagglutinins on the membranes of infected host cells. Hemagglutinins are viral surface glycoproteins that bind specifically to sialic acid residues present on RBC membranes.
When RBCs are added to a monolayer of virus-infected cells, they adhere to the cell surface due to hemagglutinin-RBC interactions, forming a visible RBC layer. This phenomenon is known as hemadsorption.
Steps in the Principle
- Viral Infection of Cells: Viruses expressing hemagglutinins replicate inside host cells and incorporate these glycoproteins into the host cell membrane.
- Addition of RBCs: When introduced into the system, they bind to the hemagglutinins, causing them to stick to infected cells.
- Microscopic Examination: The adsorbed RBCs indicate a positive HAD test, confirming viral infection.
This test distinguishes between infected and non-infected cells because normal (uninfected) cells do not express hemagglutinins and thus do not adsorb RBCs.
Procedure
The Hemadsorption Assay involves multiple steps, including cell culture preparation, viral infection, RBC treatment, and microscopic examination.
A. Preparation of Cell Culture
- Cell Line Selection: Choose a susceptible cell line, such as Vero cells, MDCK (Madin-Darby Canine Kidney) cells, or LLC-MK2 cells, which support the replication of hemagglutinating viruses.
- Cell Growth: Grow cells in Dulbecco’s Modified Eagle Medium (DMEM) or Eagle’s Minimum Essential Medium (EMEM) supplemented with fetal bovine serum (FBS) and antibiotics.
- Cell Seeding: Seed cells into tissue culture plates or flasks and incubate until a confluent monolayer is formed.
B. Viral Infection
- Virus Inoculation: Infect the monolayer with a suspected viral sample and incubate under optimal conditions (37°C in a CO₂ incubator).
- Observation Period: Allow the virus to replicate for 24–48 hours while monitoring for any cytopathic effects (CPE).
C. Hemadsorption Assay
- Washing Step: Remove the growth medium and wash the monolayer with phosphate-buffered saline (PBS) to eliminate free viral particles.
- Addition of RBC Suspension: Prepare freshly washed RBCs (typically from guinea pigs, chickens, or humans) and overlay them onto the cell monolayer.
- Incubation: Keep the culture at 4°C for 30 minutes to allow hemadsorption to occur.
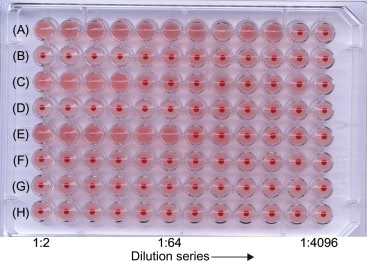
- Rinse and Observation: Gently rinse the cells with PBS and examine them under an inverted microscope.
- Result Interpretation:
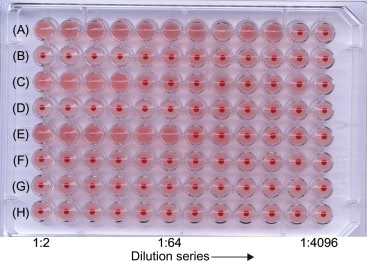
- Positive HAD Test → RBCs adhere to infected cells, forming a red layer.
- Negative HAD Test → No RBC adherence; RBCs settle at the bottom of the well.
Advantages of Hemadsorption Assay
The HAD assay is widely used for its multiple advantages, making it an essential tool in virology.
1. Rapid and Simple
- The HAD assay provides quick results within a few hours after RBC addition.
- It does not require complex equipment or expensive reagents, making it accessible in most laboratories.
2. Cost-Effective
- Compared to molecular methods like PCR (Polymerase Chain Reaction) or ELISA, HAD is a low-cost diagnostic test.
- The main materials needed are cell culture, RBCs, and a light microscope, making it ideal for resource-limited settings.
3. Does Not Require Cell Lysis
- Unlike plaque assays or lysis-based tests, the HAD method preserves the infected cell monolayer.
- This makes it possible to perform further confirmatory tests on the same culture.
4. Useful for Detecting Non-Cytopathic Viruses
- Some viruses, such as Parainfluenza or Mumps, do not cause clear cytopathic effects (CPE) in cell cultures.
- HAD enables virus detection in such cases by identifying hemagglutinin expression rather than relying on visible cell damage.
5. Applicable for Several Viruses
- HAD is useful for detecting a wide range of hemagglutinating viruses, including:
- Influenza virus
- Parainfluenza virus
- Measles virus
- Mumps virus
- Newcastle disease virus
Disadvantages of Hemadsorption Assay
Despite its advantages, HAD has some limitations that may affect its diagnostic application.
1. Requires Live Cell Cultures
- HAD can only be performed in actively growing cell cultures requiring careful maintenance.
- Not all laboratories have facilities for cell culture work, limiting the assay’s accessibility.
2. Limited to Certain Viruses
- HAD is not a universal test; it only works for viruses that express hemagglutinins.
- Non-hemagglutinating viruses (e.g., HIV, Hepatitis B, Rabies) cannot be detected using this method.
3. Time-Consuming
- Although the test is relatively quick, virus incubation takes 24–48 hours before the HAD assay can be performed.
- Other molecular methods, such as RT-PCR, can provide faster results.
4. Requires a Microscope
- The test requires an inverted microscope, which may not be available in all laboratory settings.
Limitations of Hemadsorption Assay
While the HAD assay is effective, it has some notable limitations:
- Does Not Quantify Viral Load
- The test can confirm the presence of a virus, but it does not measure viral concentration.
- Additional techniques (e.g., plaque assay, qPCR) are needed for viral quantification.
- False Negatives Possible
- Some viral strains may produce low levels of hemagglutinins, leading to false-negative results.
- Poor RBC selection or improper incubation can also affect test sensitivity.
- Does Not Differentiate Viral Strains
- The assay detects viral presence but does not identify specific strains.
- Additional tests, such as Hemagglutination Inhibition (HAI) or PCR, are needed for strain typing.
- Dependent on RBC Source
- Different species’ RBCs may show varying sensitivity to viral hemagglutinins.
- For accurate results, selecting the appropriate RBC type for the tested virus is important.