- Exfoliative cytology studies of cells that are shed or scraped from body surfaces.
- It is a non-invasive diagnostic technique primarily used for detecting abnormalities, particularly in epithelial tissues.
- In female genital tract health, exfoliative cytology is pivotal in diagnosing conditions like infections, inflammation, pre-cancerous lesions, and cancers.
- The procedure has been refined over the decades to include Pap smears and other cytological screenings that can detect early-stage abnormalities in cervical and other reproductive tract tissues, helping in early intervention and management.
-
Introduction to Exfoliative Cytology
-
- Definition and Scope: Exfoliative cytology refers to the microscopic examination of cells that are naturally shed or deliberately removed from the epithelial surfaces of organs. The technique assesses cellular health, identifying abnormalities, including infections, pre-cancerous changes, and malignancies.
- Historical Background: The origins trace back to the 1920s with Dr. George Papanicolaou’s work on cervical cancer detection. His invention of the Pap smear test revolutionized cervical cancer screening and helped reduce cervical cancer mortality.
- Clinical Significance: Exfoliative cytology is widely used due to its non-invasive nature, cost-effectiveness, and ability to detect early-stage abnormalities. It is particularly valuable in mass screening programs for cervical cancer, which rely on early detection for improved outcomes.
-
Techniques in Exfoliative Cytology
-
- Sampling Methods:
- Scraping or Brushing: A brush or spatula scrapes the cervical cells from the surface and the transformation zone.
- Swabbing: Common in other body regions where cells are more easily collected with a swab, such as the oral cavity.
- Washing: Fluids wash off cells in organs like the lungs and urinary tract.
- Types of Samples: Includes cells from the superficial and intermediate layers of epithelial tissues, focusing on areas prone to abnormalities, such as the cervix.
- Staining Techniques:
- Papanicolaou Stain: Provides differential staining to highlight cellular details and nuclei, aiding in identifying dysplasia and malignancy.
- Hematoxylin and Eosin (H&E): Common for general histology but less sensitive for cytological nuances.
- Special Stains: Periodic Acid-Schiff (PAS), Gram stain, and others help differentiate fungal organisms, bacteria, or glycogen in cells.
- Sampling Methods:
-
Female Genital Tract Anatomy and Relevance in Cytology
-
- Overview of Anatomy: The female genital tract includes the vulva, vagina, cervix, uterus, fallopian tubes, and ovaries. The cervix is a key focus area due to its accessibility and role in cervical cancer screening.
- Focus on the Cervix:
- Transformation Zone: The region between the exocervix (squamous cells) and endocervix (columnar cells) is most susceptible to HPV infection and neoplastic changes.
- Squamocolumnar Junction: A critical area in cervical cytology as dysplasia and pre-cancerous lesions are likely to originate.
- Cytological Variability in Different Genital Tract Regions: Vaginal and endometrial cells have distinct appearances, and each must be identified accurately to diagnose abnormalities specific to each site.
-
Pap Smear Test as a Model of Exfoliative Cytology
-
- Development of the Pap Smear: Introduced by Dr. George Papanicolaou in the early 20th century, it remains the gold standard in cervical cancer screening.
- Procedure for a Pap Smear:
- Sample Collection: A small brush or spatula collects cells from the cervix and the transformation zone.
- Fixation and Slide Preparation: Cells are spread on a glass slide and fixed immediately to prevent drying artifacts.
- Staining and Examination: Cells are stained and examined under a microscope for abnormal morphology using the Papanicolaou stain.
- Reporting: The Bethesda system classifies findings as normal, atypical, or indicative of specific lesions like LSIL (Low-grade squamous intraepithelial lesion), HSIL (High-grade intraepithelial lesion), or carcinoma.
-
Applications and Interpretation in Female Genital Tract Cytology
-
- Normal Cytology:
- Healthy Cervical Cells: Baseline cell populations, including superficial, intermediate, and parabasal cells.
- Hormonal Influence: Changes in cellular appearance due to hormonal fluctuations across menstrual cycles and life stages.
- Benign Cellular Changes:
- Inflammatory and Reactive Changes: The presence of inflammatory cells, such as neutrophils, indicative of benign conditions or infections.
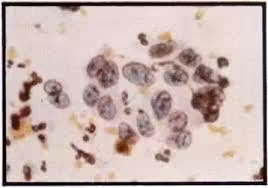
- Infections: Cellular changes caused by organisms like Trichomonas vaginalis (pear-shaped trophozoites), Candida (yeast cells), and Herpes simplex virus (multinucleation and chromatin molding).
- Hormonal Influence on Cells: Changes in vaginal and cervical cells due to estrogen or progesterone, noticeable during pregnancy, menopause, and hormonal therapy.
- Abnormal and Dysplastic Changes:
- Dysplasia: Disordered cell growth that can precede malignancy. Dysplasia is classified into LSIL and HSIL based on severity.
- Pre-Cancerous Lesions: Cytologic markers include nuclear enlargement, hyperchromasia, irregular cell borders, and increased nuclear-to-cytoplasmic ratio.
- Malignant Changes:
- Carcinoma Indicators: Larger, irregular, hyperchromatic nuclei and irregular borders. Cytologists look for clusters of abnormal cells, disordered architecture, and additional features indicative of invasive carcinoma.
- Normal Cytology:
-
The Role of Cytology in Cervical Cancer Screening and Prevention
-
- Epidemiology of Cervical Cancer: HPV is a primary risk factor, particularly strains like HPV-16 and HPV-18. Regular cytological screening significantly reduces cervical cancer incidence and mortality.
- Screening Protocols:
- Frequency of Screening: Guidelines vary by age and risk factors but typically involve biennial to triennial Pap tests.
- Co-testing with HPV: Cytology combined with HPV testing increases sensitivity for detecting high-risk HPV and pre-cancerous changes, aiding in early intervention.
- HPV Vaccination and Prevention: HPV vaccines play a major role in preventing cervical cancer, and cytology helps track the impact of vaccination programs on cervical health.
-
Advantages and Limitations of Exfoliative Cytology
-
- Advantages:
- Non-Invasive and Cost-Effective: The procedure is relatively painless and less costly than tissue biopsy.
- Effective for Mass Screening: It is widely used in screening programs due to its ability to detect early pre-cancerous and cancerous changes.
- Limitations:
- Sampling Errors: The quality of samples may vary due to insufficient cell collection, improper technique, or the presence of blood and mucus.
- Interpretation Challenges: Borderline or atypical findings may require additional testing for clarification, as cytology alone may miss certain lesions.
- Sensitivity and Specificity: While effective, exfoliative cytology does not always detect all early-stage cancers or high-risk changes, especially when using conventional smear methods without additional molecular tests.
- Advantages:
-
Recent Advances and Future Directions in Cytology
-
- Liquid-Based Cytology (LBC): Offers a more efficient alternative to conventional smears by suspending cells in a liquid medium, providing clearer samples with less debris, and facilitating further molecular testing.
- Digital Cytology and Artificial Intelligence: Automated image analysis and AI-driven software can enhance diagnostic accuracy, reduce human error, and streamline interpretation, particularly useful in large-scale screening.
- Molecular Testing and Biomarkers:
- HPV Genotyping: Identifying high-risk HPV types aids in risk stratification and helps clinicians decide on follow-up actions.
- Biomarkers for Cell Cycle and Cancer Pathways: Investigating proteins like p16 and Ki-67 in cytology samples may improve the identification of true pre-cancerous lesions.