Introduction
-
Klinefelter Syndrome (KS) is a chromosomal disorder affecting males, caused by the presence of one or more extra X chromosomes in their cells — the most common form being 47, XXY.
-
The condition leads to testicular underdevelopment (hypogonadism), infertility, and hormonal imbalance due to reduced testosterone levels.
-
It was first described by Dr. Harry Klinefelter in 1942 at Massachusetts General Hospital, when he studied a group of men with gynecomastia, small testes, and infertility.
-
It is a major genetic cause of male infertility and one of the most common chromosomal abnormalities in humans.
-
Most affected individuals are unaware of their condition until adulthood or evaluation for infertility.
Genetic Basis and Mechanism
| Aspect | Description |
|---|---|
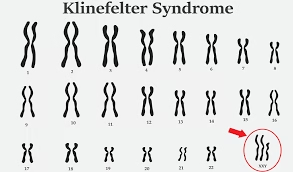
| Chromosomal pattern | 47, XXY (most common) |
| Variants | 48, XXXY; 48, XXYY; Mosaic 46,XY/47,XXY |
| Sex affected | Males only |
| Type of genetic error | Nondisjunction (failure of chromosomes to separate during meiosis) |
| Inheritance pattern | Usually sporadic (not inherited) |
| Incidence | 1 in 500–1,000 male births worldwide |
🔹 How it Happens
-
During meiosis, sex chromosomes (X and Y) fail to separate properly → sperm or egg carries an extra X chromosome.
-
When such a gamete combines with a normal gamete at fertilization, the resulting zygote has 47 chromosomes (XXY) instead of 46 (XY).
-
The presence of the extra X chromosome causes overexpression of certain X-linked genes that interfere with testicular development and hormone production.
Pathophysiology
1. Testicular Changes
-
Seminiferous tubules undergo fibrosis and hyalinization → leading to small, firm testes.
-
Leydig cell dysfunction → decreased testosterone synthesis.
-
Impaired spermatogenesis → azoospermia (absence of sperm).
2. Hormonal Feedback
-
↓ Testosterone → loss of negative feedback to the hypothalamus → ↑ release of GnRH → ↑ FSH and LH (hypergonadotropic hypogonadism).
3. Developmental Effects
-
Low testosterone levels during puberty cause incomplete masculinization, poor secondary sexual characteristics, and gynecomastia.
Epidemiology
| Feature | Details |
|---|---|
| Prevalence | 1 in every 700 male births |
| Age at diagnosis | Often during puberty or adulthood (when fertility issues appear) |
| Maternal age factor | Risk increases slightly in older mothers (>35 years) |
| Inheritance | Usually new mutation; very rarely inherited |
Clinical Features
Klinefelter’s Syndrome presents a spectrum of symptoms, from mild to severe, depending on the number of extra X chromosomes and mosaicism.
A. Physical Characteristics
| System / Feature | Findings |
|---|---|
| Height | Tall with long arms and legs (eunuchoid body habitus) |
| Shoulders and hips | Narrow shoulders, broad hips (feminine body shape) |
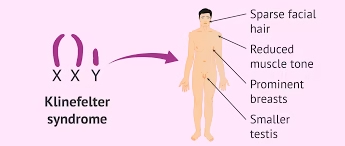
| Facial and body hair | Sparse beard, reduced chest and pubic hair |
| Muscles | Weak muscles, low tone (hypotonia in infancy) |
| Breasts | Gynecomastia in 30–50% (risk of breast cancer ↑ 20-fold compared to normal men) |
| Testes | Small, firm, nonfunctional (testicular atrophy) |
| Penis | Normal or slightly small |
| Voice | High-pitched voice |
| Bones | Osteopenia and osteoporosis due to low testosterone |
B. Reproductive and Hormonal Features
| Aspect | Effect |
|---|---|
| Testosterone | ↓ Low (hypogonadism) |
| FSH, LH | ↑ Increased (due to loss of negative feedback) |
| Sperm count | Azoospermia or severe oligospermia |
| Fertility | Usually infertile, but rare fertility possible in mosaic types |
| Sexual characteristics | Poorly developed secondary sexual traits |
| Libido | Decreased sexual drive |
C. Cognitive and Behavioural Features
| Domain | Observation |
|---|---|
| Intelligence | Usually normal, but slightly reduced (IQ 85–90) |
| Language skills | Delayed speech and language learning |
| School performance | Poor reading and writing skills (dyslexia common) |
| Personality | Shy, quiet, introverted, low confidence |
| Behavioral problems | Depression, anxiety, low self-esteem in adolescence |
D. Associated Medical Conditions
| System | Complication |
|---|---|
| Endocrine | Type 2 diabetes mellitus, metabolic syndrome |
| Cardiovascular | Venous ulcers, varicose veins, thrombosis risk |
| Skeletal | Osteoporosis due to long-term hypogonadism |
| Neoplastic | Breast cancer, extragonadal germ cell tumors |
| Dental | Taurodontism (large pulp chambers) |
| Musculoskeletal | Flat feet, scoliosis |
Diagnosis
1. Clinical Clues
-
Small, firm testes
-
Gynecomastia
-
Tall stature
-
Delayed puberty or infertility
2. Laboratory Investigations
| Test | Finding |
|---|---|
| Karyotyping | Confirms extra X chromosome (47, XXY) |
| Serum testosterone | ↓ Decreased |
| Serum LH and FSH | ↑ Increased |
| Semen analysis | Azoospermia or very low sperm count |
| Chromatin study | Barr body present (one per cell in males) |
| Bone density (DEXA scan) | Reduced |
| Hormonal profile | Low testosterone, high estrogen:testosterone ratio |
3. Imaging
-
Testicular ultrasound: small, fibrotic testes.
-
Mammography: for gynecomastia or suspected breast cancer.
-
Bone density scan: evaluates osteoporosis risk.
Differential Diagnosis
| Condition | Main Difference |
|---|---|
| Turner’s Syndrome (45,X) | Affects females; short stature, streak ovaries |
| Kallmann Syndrome | Hypogonadism with anosmia, normal karyotype (46,XY) |
| Androgen Insensitivity Syndrome | Phenotypically female with XY genotype |
| Primary testicular failure | Chromosome number normal (46,XY) |
Management and Treatment
Although there is no cure, proper hormonal therapy and multidisciplinary support can ensure a normal life.
1. Hormone Replacement Therapy
| Therapy | Purpose |
|---|---|
| Testosterone replacement | Initiated at puberty to develop secondary sexual traits |
| Benefits | Increases muscle mass, facial hair, libido, bone density, and self-esteem |
| Forms available | Injections, skin patches, gels, or oral forms |
| Monitoring | Regular check of testosterone, lipid profile, liver function, and bone density |
2. Fertility Support
-
Though infertility is common, testicular sperm extraction (TESE) combined with intracytoplasmic sperm injection (ICSI) may help some mosaic-type men become fathers.
-
Sperm banking (if possible early in life) is recommended.
3. Surgical and Medical Care
| Condition | Treatment |
|---|---|
| Gynecomastia | Cosmetic surgery or anti-estrogen drugs (tamoxifen) |
| Osteoporosis | Calcium and vitamin D, bisphosphonates if needed |
| Metabolic problems | Weight control, diet, regular exercise |
| Psychological issues | Counseling, therapy, and support groups |
4. Educational and Psychological Support
-
Speech therapy: improves communication and vocabulary
-
Special education: helps overcome learning difficulties
-
Behavioural therapy: boosts self-esteem and confidence
-
Vocational training: helps adapt to social and work environments
5. Genetic Counselling
| Purpose | Details |
|---|---|
| Family awareness | Explains genetic cause and reproductive risk |
| Recurrence risk | Usually low (sporadic cases) |
| Prenatal diagnosis | Amniocentesis or chorionic villus sampling (CVS) can detect XXY karyotype |
| Future family planning | Informed decisions and emotional preparation |
Prognosis
| Aspect | Outcome |
|---|---|
| Life expectancy | Normal with treatment |
| Fertility | Most remain infertile, but ART may help |
| Physical health | Improves significantly with testosterone therapy |
| Cognitive function | Stable with educational help |
| Mental health | Good with counseling and support |
Prevention
-
No known prevention, as it is a random chromosomal error.
-
Prenatal testing can identify cases early in pregnancy.
-
Genetic counseling helps families understand and prepare for management.
MCQs
-
Klinefelter’s Syndrome occurs in:
A. Females
B. Males
C. Both males and females
D. Only in newborns -
Klinefelter’s Syndrome is a result of:
A. Monosomy
B. Trisomy of sex chromosomes
C. Deletion
D. Translocation -
The karyotype of classical Klinefelter’s Syndrome is:
A. 45, X
B. 47, XXY
C. 47, XYY
D. 46, XY -
Klinefelter’s Syndrome is caused by:
A. Nondisjunction of sex chromosomes
B. Gene mutation
C. Translocation
D. Chromosomal deletion -
Which of the following is true about Klinefelter’s Syndrome?
A. It affects only females
B. It affects only males
C. It affects both sexes equally
D. It affects children only -
The presence of a Barr body in a male cell indicates:
A. Normal male
B. Klinefelter’s Syndrome
C. Turner’s Syndrome
D. Down’s Syndrome -
The extra chromosome in Klinefelter’s Syndrome is:
A. X chromosome
B. Y chromosome
C. Chromosome 21
D. Chromosome 13 -
Klinefelter’s Syndrome was first described by:
A. Watson and Crick
B. Jerome Lejeune
C. Harry Klinefelter
D. Turner -
The most common cause of male hypogonadism is:
A. Klinefelter’s Syndrome
B. Turner’s Syndrome
C. Down’s Syndrome
D. Fragile X Syndrome -
Which of the following is not a feature of Klinefelter’s Syndrome?
A. Tall stature
B. Gynecomastia
C. Small testes
D. Short stature -
Which hormone is decreased in Klinefelter’s Syndrome?
A. FSH
B. LH
C. Testosterone
D. Estrogen -
Which hormones are increased in Klinefelter’s Syndrome?
A. FSH and LH
B. Testosterone and LH
C. Estrogen and testosterone
D. Progesterone and LH -
Which of the following features is seen in Klinefelter’s Syndrome?
A. Short stature
B. Sparse body hair
C. Deep voice
D. Large testes -
What is the typical voice characteristic in Klinefelter’s males?
A. Deep and masculine
B. Normal
C. High-pitched voice
D. Very loud voice -
Which of the following best describes the body build of a Klinefelter male?
A. Obese with short limbs
B. Tall with long legs and narrow shoulders
C. Muscular and broad-shouldered
D. Short and stocky -
Which of the following statements about fertility is true in Klinefelter’s Syndrome?
A. Normal fertility
B. Reduced fertility
C. Complete infertility (usually)
D. Increased fertility -
Klinefelter’s Syndrome represents:
A. Female with Y chromosome
B. Male with extra X chromosome
C. Female with extra chromosome 21
D. Male with chromosome 21 trisomy -
Which of the following is a common reproductive finding?
A. Azoospermia
B. Polycystic testes
C. Increased sperm motility
D. Hyperfunctioning Leydig cells -
The testes in Klinefelter’s Syndrome are:
A. Normal-sized
B. Small and firm
C. Large and soft
D. Absent -
Klinefelter’s Syndrome results in:
A. Hypogonadotropic hypogonadism
B. Hypergonadotropic hypogonadism
C. Normal gonadal function
D. Hypergonadism -
The presence of one Barr body in a male indicates:
A. 46,XY
B. 47,XXY
C. 48,XXXY
D. 45,X -
Which of the following is a hallmark clinical finding?
A. Small, hard testes
B. Large testes
C. Undescended testes
D. Painful testes -
Which of the following is increased in serum of Klinefelter’s patients?
A. Testosterone
B. FSH
C. Cortisol
D. Insulin -
Which of the following is decreased in Klinefelter’s Syndrome?
A. Estrogen
B. Testosterone
C. LH
D. FSH -
The commonest chromosomal abnormality leading to male infertility is:
A. Turner’s Syndrome
B. Klinefelter’s Syndrome
C. Down’s Syndrome
D. Edward’s Syndrome -
The voice of Klinefelter’s males is:
A. Low-pitched
B. High-pitched
C. Normal
D. Absent -
Klinefelter’s Syndrome is detected by:
A. FISH test
B. Karyotyping
C. Blood sugar test
D. CT scan -
Which of the following is a typical mental feature?
A. Hyperactivity
B. Learning difficulty, especially in language
C. Very high IQ
D. Aggressive behavior -
Which of the following is a common dental feature?
A. Taurodontism
B. Hypodontia
C. Supernumerary teeth
D. Microdontia -
What is the typical body hair pattern in Klinefelter’s males?
A. Thick body hair
B. Sparse facial and body hair
C. Dense beard
D. Normal hair distribution -
Which of the following is a long-term complication?
A. Osteoporosis
B. Hypercalcemia
C. Polycythemia
D. Hyperthyroidism -
What is the risk of breast cancer in Klinefelter’s males compared to normal males?
A. No risk
B. Equal risk
C. Increased 20-fold
D. Decreased -
Testosterone therapy in Klinefelter’s Syndrome improves all except:
A. Muscle mass
B. Libido
C. Height
D. Bone density -
Which type of nondisjunction causes Klinefelter’s Syndrome?
A. Meiotic
B. Mitotic
C. Both meiotic and mitotic
D. Postzygotic deletion -
The definitive diagnostic test for Klinefelter’s Syndrome is:
A. Blood test for testosterone
B. FSH estimation
C. Karyotype analysis
D. Ultrasound of testes
Answer Key
-
B — Males
-
B — Trisomy of sex chromosomes
-
B — 47, XXY
-
A — Nondisjunction of sex chromosomes
-
B — It affects only males
-
B — Klinefelter’s Syndrome
-
A — X chromosome
-
C — Harry Klinefelter
-
A — Klinefelter’s Syndrome
-
D — Short stature
-
C — Testosterone
-
A — FSH and LH
-
B — Sparse body hair
-
C — High-pitched voice
-
B — Tall with long legs and narrow shoulders
-
C — Complete infertility (usually)
-
B — Male with extra X chromosome
-
A — Azoospermia
-
B — Small and firm
-
B — Hypergonadotropic hypogonadism
-
B — 47, XXY
-
A — Small, hard testes
-
B — FSH
-
B — Testosterone
-
B — Klinefelter’s Syndrome
-
B — High-pitched
-
B — Karyotyping
-
B — Learning difficulty, especially in language
-
A — Taurodontism
-
B — Sparse facial and body hair
-
A — Osteoporosis
-
C — Increased 20-fold
-
C — Height
-
C — Both meiotic and mitotic
-
C — Karyotype analysis