Leishmania is a genus of parasitic protozoa responsible for a group of diseases collectively known as leishmaniasis. These diseases are transmitted by biting infected sandflies. They can cause a range of clinical manifestations, from cutaneous (skin lesions) to visceral (internal organ involvement) and mucocutaneous forms.
Habitat
Leishmania parasites have a heteroxenous life cycle, meaning they require two distinct hosts for their complete development:
- Invertebrate Host (Vector): The female sandfly is the vector that transmits the parasite. The sandfly typically bites mammals, including humans, for blood meals.
- Vertebrate Host: The mammalian host, including humans, dogs, and rodents, provides the environment where the parasite undergoes part of its lifecycle.
Leishmania parasites live and multiply in different tissues depending on the form of leishmaniasis:
- Cutaneous Leishmaniasis: Primarily affects the skin, causing lesions or ulcers.
- Visceral Leishmaniasis (Kala-azar): Primarily affects internal organs, such as the spleen, liver, and bone marrow.
- Mucocutaneous Leishmaniasis: Affects both the mucous membranes and skin.
Epidemiology
- Global Distribution: Leishmaniasis is found in tropical, subtropical, and temperate regions. It affects approximately 12 million people worldwide, with an estimated 1.5 million new cases yearly. The highest incidence is in parts of South America, Africa, Asia, and the Mediterranean.
- Endemic Areas: Leishmaniasis is endemic in over 80 countries, particularly India, Brazil, Afghanistan, Sudan, Ethiopia, Bangladesh, and Latin America.
- At-Risk Populations: People living in rural areas, particularly those with poor sanitation, overcrowded conditions, and malnutrition, are at higher risk. Immunocompromised individuals (e.g., those with HIV/AIDS) are also at greater risk for more severe forms of leishmaniasis.
- Transmission: The disease is transmitted through the bite of an infected female sandfly, the vector. The sandfly becomes infected after biting an infected mammalian host and acquiring the promastigote form of the parasite.
Morphology
Leishmania exists in two distinct forms during its life cycle:
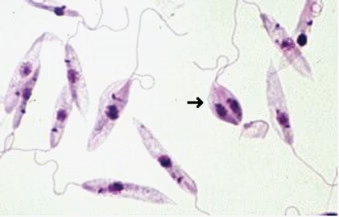
- Promastigote (vector form):
- The promastigote is the flagellated, extracellular, motile form found in the gut of the sandfly vector.
- It has a long body with a prominent flagellum extending from the anterior end.
- The kinetoplast, a structure containing mitochondrial DNA, is located at the base of the flagellum.
- Promastigotes are adapted for survival in the sandfly’s midgut.
- Amastigote (host form):
- The amastigote is the non-flagellated, intracellular form of Leishmania found within macrophages in the mammalian host.
- Amastigotes are round or oval and contain a small kinetoplast and a nucleus.
- This form is responsible for multiplying within the host cells, replicating by binary fission.
Life Cycle
The life cycle of Leishmania is heteroxenous and involves two hosts: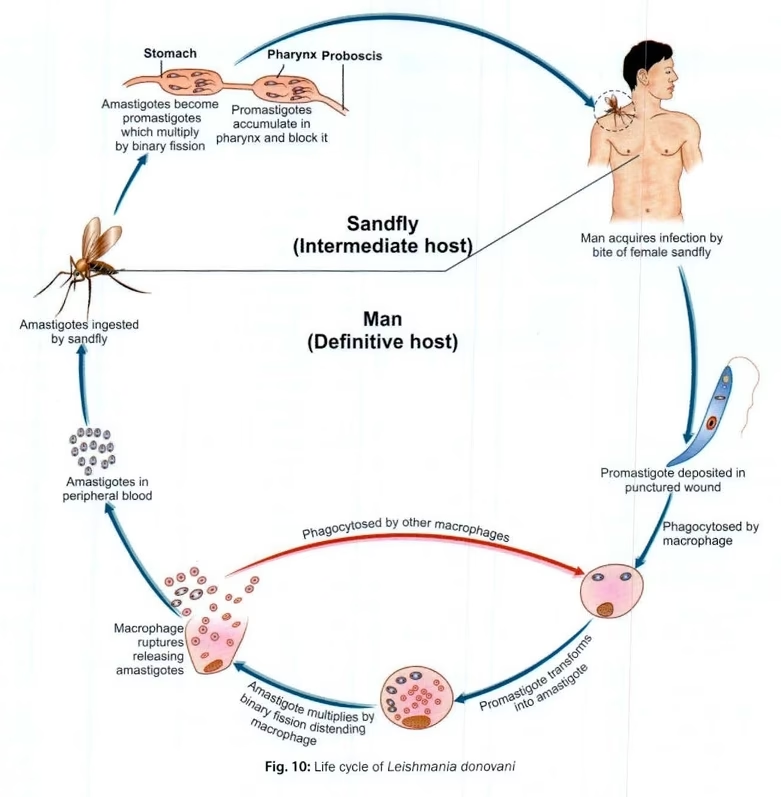
- In the Vector (Sandfly):
- The sandfly takes up promastigotes when it feeds on an infected mammalian host.
- Inside the sandfly’s midgut, the promastigotes divide and transform into the infective form (flagellated promastigotes).
- The promastigotes migrate to the proboscis (mouthparts) of the sandfly.
- In the Host (Mammal):
- When the infected sandfly bites a mammal, it injects promastigotes into the skin.
- Once inside the mammalian body, the promastigotes are engulfed by macrophages (a type of white blood cell).
- Inside the macrophages, the promastigotes transform into amastigotes, the non-flagellated form.
- The amastigotes multiply within the macrophages by binary fission, eventually causing the macrophage to rupture and release the amastigotes into the surrounding tissue.
- The cycle continues as new sandflies become infected by feeding on an infected mammalian host.
- Transmission to the Next Host:
- When an uninfected sandfly bites an infected mammal, it ingests amastigotes.
- Inside the sandfly’s gut, the amastigotes transform into promastigotes, which then move to the proboscis of the sandfly, ready to infect the next host.
Pathogenesis
The pathogenesis of Leishmania infection depends on the species of Leishmania, the host’s immune status, and the form of leishmaniasis (cutaneous, visceral, or mucocutaneous).
- Host Immunity: The parasite primarily infects macrophages, evading the host immune system by inhibiting lysosomal killing inside the macrophage and replicating inside these cells.
- Inflammation: The host responds by activating an immune response, including releasing cytokines and inflammatory mediators. This can lead to skin ulcers (in cutaneous leishmaniasis) or enlargement of organs like the liver and spleen (in visceral leishmaniasis).
- Chronic Infection: In chronic cases, the infection can lead to tissue destruction, organ failure, and immune suppression.
- Visceral Leishmaniasis (Kala-azar):
- Tissues affected: Primarily affects the liver, spleen, bone marrow, and intestines.
- The disease causes fever, weight loss, anemia, and splenomegaly (spleen enlargement).
- Immunocompromised individuals, including those with HIV/AIDS, are at higher risk of severe visceral leishmaniasis.
- Cutaneous Leishmaniasis:
- Characterized by the formation of skin ulcers at the site of the sandfly bite.
- Lesions are often self-limiting but can lead to scarring and disfigurement.
- Mucocutaneous Leishmaniasis:
- This disease affects the skin and mucous membranes, particularly in the nose, mouth, and throat. It can cause severe mucosal destruction.
Laboratory Diagnosis
Diagnosis of Leishmania infections typically involves clinical assessment, microscopic examination, and serological tests.
Microscopy:
- Direct examination of lesion material (e.g., skin ulcers or aspirates from enlarged spleen/liver) can reveal amastigotes inside macrophages.
- Staining methods such as Giemsa stain can visualize the amastigotes in smears from biopsy specimens, aspirates, or scrapings.
Culture:
- Leishmania parasites can be cultured in NNN (Novy-MacNeal-Nicolle) or RPMI medium. This helps to grow promastigotes from tissue samples or blood.
Serology:
- Enzyme-linked immunosorbent assay (ELISA) or direct agglutination test (DAT) can be used to detect specific antibodies against Leishmania species in the serum of infected individuals.
- PCR-based methods are increasingly used for species identification and detection of Leishmania DNA.
Molecular Techniques:
- Polymerase Chain Reaction (PCR) can detect Leishmania DNA in clinical samples and identify the species responsible for the infection.
- PCR is also used to quantify parasites, particularly in visceral leishmaniasis.
Skin Test:
- A Montenegro skin test (similar to a tuberculosis skin test) can detect delayed-type hypersensitivity to Leishmania antigens, though it is not specific to the infection.