- Neuropathology techniques involve specialized methodologies for examining central and peripheral nervous system tissues, primarily to diagnose diseases such as tumors, infections, neurodegenerative disorders, inflammatory conditions, and vascular abnormalities.
- The nervous system’s unique cellular architecture, along with the vulnerability of neuronal tissues to degradation, necessitates specialized techniques in tissue handling, fixation, staining, and imaging.
- Below, I outline key techniques in neuropathology, covering tissue preparation, staining, advanced imaging, and molecular techniques.
Tissue Collection and Preparation
The collection and preparation of nervous tissue in neuropathology are critical first steps that require meticulous attention to detail due to the sensitivity of the brain and spinal cord to autolysis and damage.
Tissue Collection Techniques
- Brain Autopsy: In post-mortem neuropathology, the brain should be removed carefully, usually by severing the cranial nerves, blood vessels, and spinal cord attachment. After removal, it’s weighed and grossly examined to document any evident abnormalities.
- Biopsy of Brain and Spinal Cord: Small brain or spinal cord biopsy samples may be taken for diagnostic purposes. Biopsies often involve a stereotactic approach for accuracy, particularly when targeting deep brain structures.
Immediate Handling and Fixation
- Time-Sensitive Fixation: Neuronal tissues degrade quickly, so tissue should be immersed in fixative as soon as possible to maintain cellular morphology.
- Fixative Choices:
- 10% Neutral Buffered Formalin is the standard for preserving morphology.
- Paraformaldehyde (4%) is common in research for better immunohistochemical labeling.
- Glutaraldehyde may be used for electron microscopy (EM) due to its strong cross-linking properties, preserving ultrastructure but often making tissue brittle.
Perfusion Fixation (primarily in research or animal models)
- This method injects fixative through the vascular system, ensuring rapid and even fixation across brain tissue. It is typically only used in research settings with animal brains to limit degradation and improve structural preservation.
Sectioning and Embedding Techniques
Sectioning nervous tissue requires specialized handling to ensure key anatomical structures are preserved and accurately represented.
Paraffin Embedding and Sectioning
- Standard Processing: After fixation, the brain tissue undergoes dehydration and is embedded in paraffin for long-term preservation.
- Section Thickness: Sections are generally cut between 4–6 µm for light microscopy, allowing visualization of cellular details without excessive overlapping of tissue layers.
- Embedding Orientation: Ensuring the correct orientation, such as aligning the hippocampus or cortex, is essential to retain the brain’s architectural layout, making diagnosis more accurate.
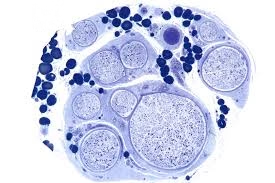
Cryostat Sectioning of Frozen Tissue
- Benefits: Frozen sections preserve enzymes, certain lipids, and cellular antigens, making them useful for enzyme histochemistry, immunohistochemistry, and immunofluorescence.
- Sectioning Procedure: Cryostat machines keep tissues frozen at -20°C to -30°C, producing sections as thin as 5 µm mounted on slides. These sections are essential in rapid diagnostic procedures, particularly during neurosurgery, where immediate diagnostic feedback is needed.
Free-Floating Sections for Immunohistochemistry
- Technique: Thicker sections (30–100 µm) are cut and kept in a buffer solution, allowing antibodies to penetrate more effectively during staining, improving results in immunohistochemistry and immunofluorescence staining for complex protein networks.
Histological Staining Techniques
Neuropathological stains highlight specific aspects of neural tissue, from general architecture to cellular subtypes and pathological features.
Hematoxylin and Eosin (H&E) Stain
Reagents:
- Hematoxylin solution
- Eosin solution
- Acid-alcohol (for differentiation)
- Tap water (for bluing)
Procedure:
- Deparaffinize sections in xylene and hydrate through a graded alcohol series.
- Stain in hematoxylin for 5–10 minutes.
- Rinse in running tap water to remove excess stains.
- Differentiate in acid-alcohol briefly, then rinse in tap water.
- Bluing in tap water or a weak alkaline solution (e.g., lithium carbonate).
- Stain with eosin for 1–2 minutes.
- Dehydrate through alcohol series, clear in xylene, and mount.
Result:
- Nuclei appear blue.
- Cytoplasm, muscle, and extracellular matrix stain varying shades of pink.
- Allows assessment of general tissue morphology, cell distribution, and necrosis.
Luxol Fast Blue (LFB) Stain
Reagents:
- Luxol Fast Blue solution
- 0.05% Lithium carbonate solution (for differentiation)
- 70% Ethanol (for further differentiation if necessary)
Procedure:
- Deparaffinize and hydrate sections.
- Stain in Luxol Fast Blue solution overnight at 60°C.
- Rinse in 95% alcohol and distilled water.
- Differentiate in lithium carbonate solution for a few seconds.
- Rinse in 70% ethanol until only myelin sheaths remain blue.
- Dehydrate, clear, and mount.
Result:
- Myelin stains blue, which helps in assessing myelination in white matter.
- Demyelinated areas appear pale or colorless, highlighting lesions as seen in multiple sclerosis and other demyelinating diseases.
Cresyl Violet (Nissl) Stain
Reagents:
- Cresyl Violet acetate solution
- Distilled water
- Alcohol series for differentiation
Procedure:
- Deparaffinize and hydrate tissue sections.
- Stain in Cresyl Violet solution for 5–10 minutes at room temperature.
- Rinse in distilled water.
- Differentiate in alcohol if needed to remove excess stains.
- Dehydrate, clear, and mount.
Result:
- Nissl substance (ribosomes in neurons) stains purple, with neuron cell bodies appearing prominently.
- Useful for assessing neuronal density and morphology, highlighting neuronal damage and loss in neurodegenerative disorders.
Bielschowsky’s Silver Stain
Reagents:
- Silver nitrate solution
- Ammonium hydroxide
- Developer (e.g., formalin)
Procedure:
- Treat sections with silver nitrate and ammonium hydroxide to form a silver solution.
- Incubate sections in the silver solution, allowing it to bind to neuronal structures.
- Develop the silver staining by adding formalin.
- Rinse in water, dehydrate, clear, and mount.
Result:
- Axons, neurofibrillary tangles, and amyloid plaques appear black or dark brown.
- Used to visualize neuronal processes, axonal abnormalities, and amyloid plaques in Alzheimer’s disease.
Gallyas Silver Stain
Reagents:
- Silver iodide solution
- Developer (e.g., formaldehyde)
Procedure:
- Apply silver iodide to sections to sensitize them.
- Wash and develop the stain with a formaldehyde-based developer.
- Dehydrate, clear, and mount.
Result:
- Tau-positive neurofibrillary tangles appear darkly stained.
- Useful in diagnosing tauopathies, especially in Alzheimer’s disease and other neurodegenerative disorders involving tau proteins.
Periodic Acid-Schiff (PAS) Stain
Reagents:
- Periodic acid solution
- Schiff reagent
- Hematoxylin for counterstaining
Procedure:
- Deparaffinize and hydrate sections.
- Treat with periodic acid for oxidation.
- Rinse and apply Schiff reagent to develop color.
- Counterstain with hematoxylin.
- Rinse, dehydrate, clear, and mount.
Result:
- Carbohydrates and glycogen stain magenta.
- Useful for detecting glycogen storage diseases, fungal infections, and basement membrane abnormalities.
Congo Red Stain
Reagents:
- Congo Red solution
- Alkaline alcohol solution for differentiation
Procedure:
- Deparaffinize and hydrate tissue sections.
- Stain in Congo Red solution for about 20 minutes.
- Differentiate with an alkaline alcohol solution.
- Rinse, dehydrate, clear, and mount.
Result:
- Amyloid deposits appear red under light microscopy and exhibit apple-green birefringence under polarized light.
- Commonly used to identify amyloid in conditions such as Alzheimer’s disease and amyloidosis.
Holzer’s Stain
Reagents:
- Crystal violet solution
- Potassium bromide solution
- Aniline-chloroform solution
Procedure:
- Stain sections with crystal violet solution.
- Differentiate using a potassium bromide solution.
- Treat with aniline-chloroform solution to remove non-specific staining.
- Dehydrate, clear, and mount.
Result:
- Glial fibers stain blue or purple.
- Useful for identifying reactive gliosis, highlighting astrocytic proliferation in response to injury or disease.
Immunohistochemistry (IHC)
Reagents:
- Primary antibodies specific to proteins of interest (e.g., GFAP, NeuN, β-amyloid, phosphorylated tau, etc.)
- Secondary antibody conjugated to an enzyme (e.g., horseradish peroxidase) or fluorophore
- Chromogen substrate (e.g., DAB) for color development
Procedure:
- Deparaffinize and rehydrate sections.
- Perform antigen retrieval if needed.
- Block non-specific binding sites with a blocking buffer.
- Incubate with a primary antibody.
- Apply a secondary antibody conjugated with an enzyme or fluorophore.
- Develop color reaction with DAB for enzyme-conjugated antibodies or visualize under fluorescence for fluorophore-labeled antibodies.
- Counterstain, if required, dehydrate, clear, and mount.
Result:
- Target proteins appear brown (DAB) or fluorescent, depending on the chromogen or fluorophore used.
- Allows identification of cell-specific markers, such as GFAP for astrocytes, β-amyloid and phosphorylated tau in Alzheimer’s, and CD68 for microglia/macrophages.
Fluorescence In Situ Hybridization (FISH)
Reagents:
- Fluorescently labeled DNA probes specific to genes of interest
- Denaturation and hybridization buffers
Procedure:
- Pre-treat and dehydrate tissue sections.
- Apply DNA probes and denature them alongside the tissue DNA.
- Hybridize the probes to the target DNA sequences in tissue.
- Wash to remove unbound probes.
- Visualize using fluorescence microscopy.
Result:
- Target DNA sequences fluoresce in specific colors, indicating gene amplification, deletions, or translocations.
- Commonly used for identifying genetic alterations in tumors, such as 1p/19q co-deletion in oligodendrogliomas.