Introduction
-
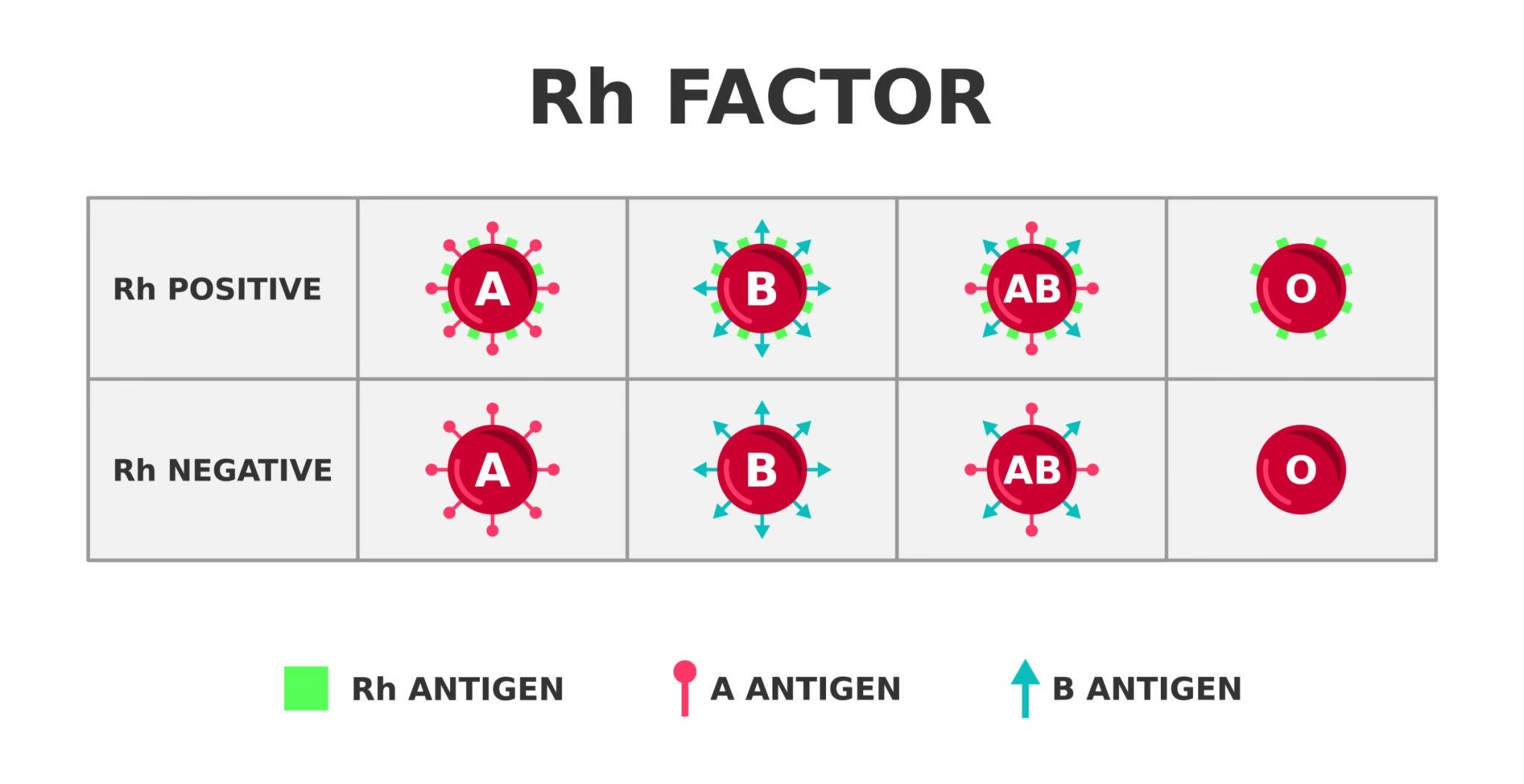
Rh blood group system is the second most important blood group system after ABO.
-
It is highly polymorphic, with more than 50 antigens identified.
-
Clinically most significant antigen: D antigen
-
Major importance in:
-
Blood transfusion reactions
-
Hemolytic disease of fetus and newborn (HDFN)
-
-
Rh antigens are protein antigens, unlike carbohydrate ABO antigens.
-
Present only on red blood cells, not in body secretions.
History
-
Discovered in 1940 by Karl Landsteiner and Alexander Wiener
-
Rabbits were immunized with Rhesus monkey red cells
-
Resulting antibodies agglutinated human red cells
-
Initially believed to be same antigen; later clarified as different but related
-
Explained:
-
Severe transfusion reactions
-
Erythroblastosis fetalis
-
-
The term “Rh factor” became widely accepted.
Genetics
-
Genes located on chromosome 1 (1p36.11)
-
Controlled by two closely linked genes:
-
RHD gene → codes for D antigen
-
RHCE gene → codes for C/c and E/e antigens
-
-
Genes are inherited as a haplotype
-
Rh positivity depends on presence of RHD gene
-
Rh negativity usually due to complete deletion of RHD gene
-
Unlike ABO:
-
No naturally occurring antibodies
-
Antibodies develop only after exposure
-
Molecular Genetics of Rh System
-
RHD and RHCE genes encode transmembrane proteins
-
Proteins have:
-
10–12 membrane-spanning segments
-
Intracellular and extracellular loops
-
-
Small amino acid substitutions cause:
-
Weak D
-
Partial D
-
Other Rh variants
-
-
Rh proteins are closely associated with:
-
Rh-associated glycoprotein (RhAG)
-
-
Normal Rh antigen expression requires:
-
Functional RHD/RHCE
-
Functional RhAG gene
-
Nature of Rh Antigens
-
Rh antigens are:
-
Proteins
-
Heat stable
-
Enzyme sensitive
-
-
Fully developed at birth
-
Not present in saliva or body fluids
-
Strongly immunogenic:
-
D antigen is one of the most immunogenic antigens known
-
-
Do not activate complement efficiently
-
Antibody-coated cells are removed by extravascular hemolysis
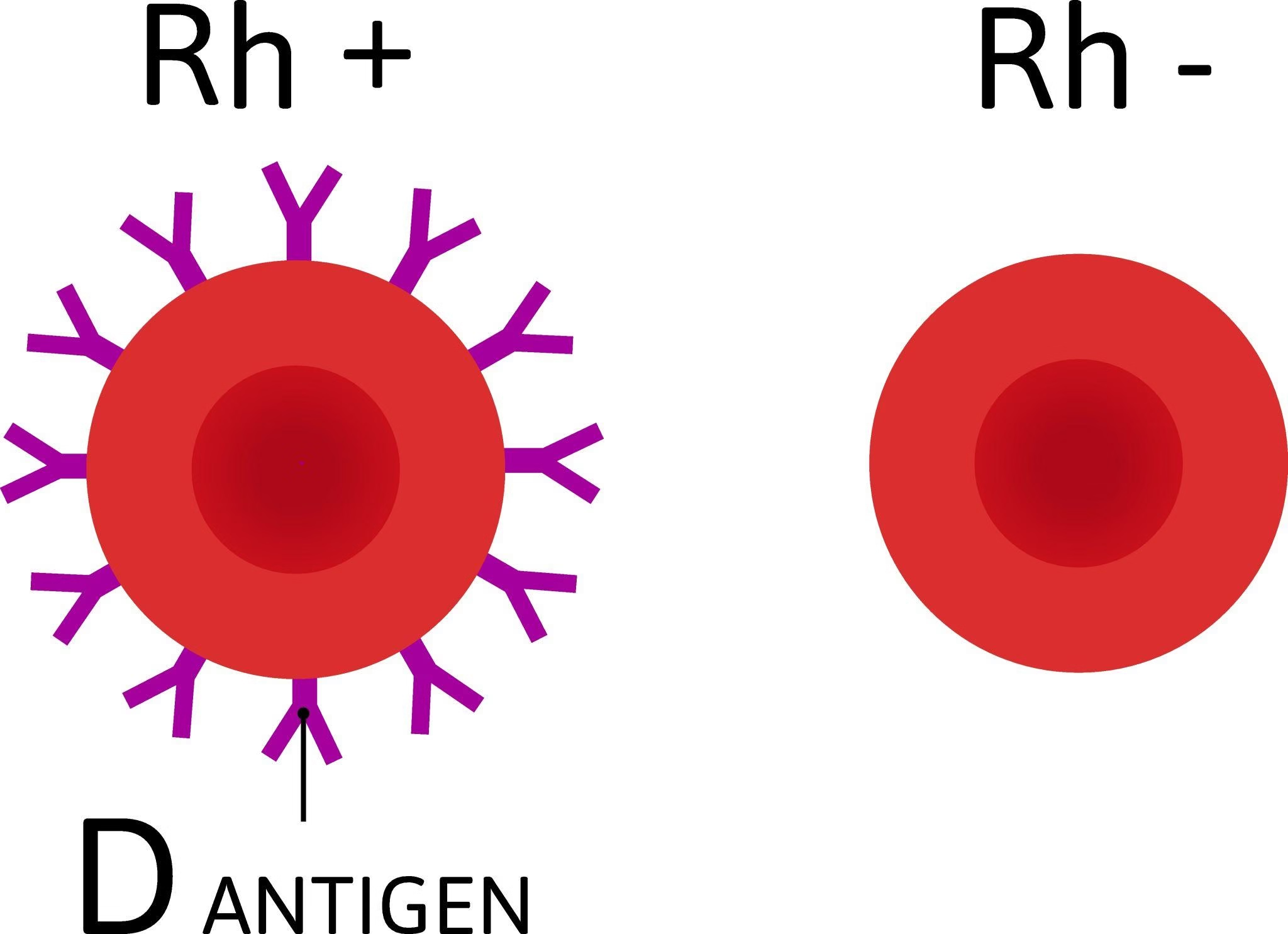
D Antigen
-
Most important antigen in Rh system
-
Present in ~85% of population
-
Highly immunogenic:
-
1 unit transfusion → ~80% chance of sensitization
-
-
Presence defines Rh positive
-
Absence defines Rh negative
-
Primary cause of:
-
Severe transfusion reactions
-
HDFN
-
Weak D (Du Antigen)
-
Reduced expression of D antigen on RBC surface
-
Caused by:
-
Amino acid substitutions in transmembrane region
-
-
Not detectable by immediate spin testing
-
Detected by:
-
Indirect Antiglobulin Test (IAT)
-
-
Characteristics:
-
D antigen complete but quantitatively reduced
-
Usually do not form anti-D
-
-
Blood bank significance:
-
Donors → treated as Rh positive
-
Recipients → often treated as Rh negative (policy dependent)
-
Partial D Antigen
-
D antigen is qualitatively incomplete
-
One or more D epitopes are missing
-
Caused by:
-
Hybrid RHD–RHCE genes
-
-
Individuals may:
-
Type as Rh positive
-
Still produce anti-D when exposed
-
-
Very important in:
-
Pregnancy
-
Transfusion medicine
-
-
Treated as Rh negative recipients
Other Variants of Rh System
-
Includes:
-
Cw, Cx, Ew
-
Del phenotype
-
Hybrid Rh antigens
-
-
Common in certain ethnic groups
-
Often undetected by routine serology
-
Require:
-
Advanced serological testing
-
Molecular genotyping
-
-
Can cause:
-
Unexpected alloimmunization
-
Delayed hemolytic reactions
-
Rh-Null Phenotype
-
Complete absence of all Rh antigens
-
Extremely rare
-
Two types:
-
Amorph type – deletion/inactivation of RHD & RHCE
-
Regulator type – mutation in RhAG gene
-
-
Clinical features:
-
Mild to moderate hemolytic anemia
-
Stomatocytosis
-
Increased RBC fragility
-
-
Transfusion problems:
-
Only Rh-null blood compatible
-
-
Demonstrates structural importance of Rh proteins
Rh Antibodies
-
Not naturally occurring
-
Formed only after:
-
Transfusion
-
Pregnancy
-
-
Belong to IgG class
-
Cross placenta easily
-
Common antibodies:
-
Anti-D (most significant)
-
Anti-C
-
Anti-E
-
Anti-c
-
-
Cause:
-
Hemolytic transfusion reactions
-
HDFN
-
-
Best detected by:
-
Indirect Coombs test
-
Factors Influencing Rh Immunization
-
Volume of antigen exposure
-
Immunogenic strength of antigen
-
Route of exposure:
-
Transfusion > pregnancy
-
-
Genetic makeup of recipient
-
ABO incompatibility:
-
Reduces Rh immunization
-
-
Frequency of exposure
-
Use or absence of anti-D prophylaxis
Functional Role of Rh Antigens
-
Not only blood group markers
-
Act as:
-
Ammonia transport channels
-
CO₂ transport facilitators
-
-
Maintain:
-
Red cell membrane stability
-
Cell shape and deformability
-
-
Loss of Rh proteins leads to:
-
Membrane defects
-
Reduced RBC survival
-
-
Explains anemia seen in Rh-null individuals
Clinical Significance of Rh System
-
Essential in:
-
Blood grouping
-
Cross-matching
-
Antenatal screening
-
-
Anti-D prophylaxis prevents:
-
HDFN
-
Maternal sensitization
-
-
Molecular Rh typing improves:
-
Transfusion safety
-
Management of complex cases
-
MCQs
1. The Rh blood group system was discovered in:
A. 1935
B. 1937
C. 1940
D. 1945
Answer: C. 1940
2. Discovery of Rh system is credited to:
A. Landsteiner and Levine
B. Wiener and Coombs
C. Landsteiner and Wiener
D. Ehrlich and Pauling
Answer: C. Landsteiner and Wiener
3. Rh blood group system is second in importance after:
A. Kell
B. ABO
C. Lewis
D. Duffy
Answer: B. ABO
4. The most immunogenic antigen of Rh system is:
A. C
B. c
C. E
D. D
Answer: D. D
5. Rh antigens are chemically:
A. Carbohydrates
B. Glycolipids
C. Proteins
D. Lipopolysaccharides
Answer: C. Proteins
6. Rh antigens are located on:
A. Plasma proteins
B. Platelets
C. Red cell membrane
D. Leukocytes
Answer: C. Red cell membrane
7. Genes controlling Rh system are located on chromosome:
A. 6
B. 9
C. 1
D. 19
Answer: C. 1
8. RHD gene encodes which antigen?
A. C
B. E
C. D
D. c
Answer: C. D
9. RHCE gene encodes which antigens?
A. D only
B. C and D
C. C/c and E/e
D. D and E
Answer: C. C/c and E/e
10. Rh-negative phenotype is usually due to:
A. Suppressed gene expression
B. Mutation of RHCE gene
C. Deletion of RHD gene
D. Absence of RhAG protein
Answer: C. Deletion of RHD gene
11. Naturally occurring antibodies are:
A. Present in Rh system
B. Absent in Rh system
C. IgM type
D. Cold reacting
Answer: B. Absent in Rh system
12. Rh antibodies are usually of which class?
A. IgM
B. IgA
C. IgE
D. IgG
Answer: D. IgG
13. Rh antibodies are formed after:
A. Birth
B. Infection
C. Sensitization
D. Vaccination
Answer: C. Sensitization
14. Which Rh antibody most commonly causes HDFN?
A. Anti-E
B. Anti-C
C. Anti-c
D. Anti-D
Answer: D. Anti-D
15. Weak D antigen is best detected by:
A. Immediate spin test
B. Saline method
C. Indirect antiglobulin test
D. Enzyme test
Answer: C. Indirect antiglobulin test
16. Weak D is caused by:
A. Missing D epitopes
B. Reduced antigen expression
C. Absence of D gene
D. ABO incompatibility
Answer: B. Reduced antigen expression
17. Individuals with weak D usually:
A. Produce anti-D
B. Do not produce anti-D
C. Always Rh negative
D. Have Rh-null phenotype
Answer: B. Do not produce anti-D
18. Partial D individuals may produce:
A. Anti-E
B. Anti-c
C. Anti-D
D. Anti-A
Answer: C. Anti-D
19. Partial D occurs due to:
A. Quantitative reduction
B. Hybrid gene formation
C. Gene deletion
D. RhAG mutation
Answer: B. Hybrid gene formation
20. Del phenotype is characterized by:
A. Absence of Rh antigens
B. Very weak D expression
C. Complete D antigen
D. Excess D antigen
Answer: B. Very weak D expression
21. Rh-null phenotype lacks:
A. Only D antigen
B. Only C and E antigens
C. All Rh antigens
D. ABO antigens
Answer: C. All Rh antigens
22. Rh-null individuals commonly show:
A. Polycythemia
B. Leukopenia
C. Hemolytic anemia
D. Thrombocytopenia
Answer: C. Hemolytic anemia
23. Rh-null regulator type is due to mutation in:
A. RHD gene
B. RHCE gene
C. RhAG gene
D. Kell gene
Answer: C. RhAG gene
24. RhAG protein is essential for:
A. ABO expression
B. Rh antigen expression
C. Platelet function
D. Complement activation
Answer: B. Rh antigen expression
25. Rh antigens are fully developed:
A. At 6 months
B. At 1 year
C. At birth
D. After puberty
Answer: C. At birth
26. Rh antigens are absent in:
A. Plasma
B. Saliva
C. Both A and B
D. Serum only
Answer: C. Both A and B
27. Main mechanism of hemolysis in Rh incompatibility is:
A. Intravascular
B. Complement mediated
C. Extravascular
D. Mechanical
Answer: C. Extravascular
28. Rh antibodies can cross placenta because they are:
A. IgM
B. IgA
C. IgE
D. IgG
Answer: D. IgG
29. ABO incompatibility reduces Rh sensitization because:
A. Rh antigens are destroyed early
B. Antibodies neutralize Rh
C. RBCs are cleared rapidly
D. Rh antibodies are IgM
Answer: C. RBCs are cleared rapidly
30. Most effective prevention of Rh immunization is:
A. Blood grouping
B. Cross matching
C. Anti-D immunoglobulin
D. Steroids
Answer: C. Anti-D immunoglobulin
31. Anti-D prophylaxis is given to:
A. Rh-positive mother
B. Rh-negative mother
C. Rh-positive fetus
D. Rh-null mother
Answer: B. Rh-negative mother
32. Rh proteins are primarily involved in transport of:
A. Oxygen
B. Sodium
C. Ammonia and CO₂
D. Glucose
Answer: C. Ammonia and CO₂
33. Absence of Rh proteins leads to:
A. Increased RBC lifespan
B. Membrane instability
C. Thrombosis
D. Leukocytosis
Answer: B. Membrane instability
34. Which Rh antigen is most common after D?
A. E
B. C
C. c
D. e
Answer: C. c
35. Rh system antibodies are best detected by:
A. Slide method
B. Tube saline method
C. Indirect Coombs test
D. Direct Coombs test
Answer: C. Indirect Coombs test
36. Rh antibodies are optimally reactive at:
A. 4°C
B. 22°C
C. 37°C
D. 60°C
Answer: C. 37°C
37. Which condition is most severe in Rh incompatibility?
A. ABO HDN
B. Rh HDN
C. Kell HDN
D. Lewis HDN
Answer: B. Rh HDN
38. Rh antigens do not activate complement efficiently because they are:
A. Carbohydrate
B. Protein antigens
C. Weak antigens
D. IgM mediated
Answer: B. Protein antigens
39. Which test is used to confirm Rh-null phenotype?
A. Slide test
B. Enzyme test
C. Molecular typing
D. Forward grouping
Answer: C. Molecular typing
40. Which Rh antigen variant poses maximum transfusion risk?
A. Weak D
B. Partial D
C. Del
D. Cw
Answer: B. Partial D
41. Rh blood group system consists of more than:
A. 10 antigens
B. 20 antigens
C. 30 antigens
D. 50 antigens
Answer: D. 50 antigens
42. Rh antibodies cause hemolysis mainly in:
A. Liver and spleen
B. Kidney
C. Blood vessels
D. Bone marrow
Answer: A. Liver and spleen
43. Rh antigen expression is restricted to:
A. All body cells
B. Epithelial cells
C. Erythroid cells
D. Platelets
Answer: C. Erythroid cells
44. Weak D differs from partial D because weak D is:
A. Qualitative defect
B. Quantitative defect
C. Complete absence
D. Gene deletion
Answer: B. Quantitative defect
45. Partial D individuals are treated as Rh-negative because they may:
A. Lack RhAG
B. Develop anti-D
C. Be Rh-null
D. Have ABO antibodies
Answer: B. Develop anti-D
46. Rh system inheritance is best described as:
A. Simple dominant
B. Simple recessive
C. Haplotypic inheritance
D. Codominant only
Answer: C. Haplotypic inheritance
47. Rh antibodies are detected during pregnancy by:
A. Forward grouping
B. Reverse grouping
C. Antibody screening
D. Cross match only
Answer: C. Antibody screening
48. Rh antigen density is highest on:
A. Fetal RBCs
B. Newborn RBCs
C. Adult RBCs
D. Reticulocytes
Answer: C. Adult RBCs
49. Rh incompatibility is most likely when mother is:
A. Rh positive
B. Rh negative
C. ABO incompatible
D. Rh-null
Answer: B. Rh negative
50. Rh blood group system is clinically important mainly because of:
A. Frequency
B. Molecular complexity
C. Immunogenicity
D. Secretor status
Answer: C. Immunogenicity