Introduction
- Bone marrow is the main factory of blood cells.
- It produces red cells, white cells, and platelets.
- Many blood diseases start in the marrow, so studying marrow samples is very important.
- When a doctor takes a bone marrow aspirate, it looks like blood mixed with small particles of marrow.
- If we see it directly under the microscope, the cells look almost transparent.
- We cannot identify them clearly. That is why staining is necessary.
- Stains give color to the cells.
- Different parts of the cell take up different colors, which helps us recognize the type of cell, its stage of development, and any abnormal changes.
Bone marrow stains are of different types:
-
Routine stains – show overall structure and all types of cells.
-
Cytochemical stains – show chemical activity in cells, used especially in leukemia.
-
Special stains – show iron, fibers, parasites, or other material.
-
Immunostains – modern method, use antibodies to detect specific cell markers.
Why do we stain bone marrow smears?
-
To see cell shape, size, and nucleus clearly.
-
To study the maturation sequence of red cells and white cells.
-
To calculate myeloid : erythroid (M:E) ratio.
-
To detect blast cells in leukemia.
-
To identify iron stores and sideroblasts.
-
To detect abnormal deposits like glycogen or lipids.
-
To find infections (parasites, fungi, TB).
-
To classify different types of leukemia.
Basic Principle of Staining
-
Acidic dyes (like eosin) color basic parts of the cell (hemoglobin, cytoplasm) → red or pink.
-
Basic dyes (like methylene blue, azure) color acidic parts (DNA, RNA) → blue or purple.
-
Romanowsky stains combine both and give polychromatic effect → multiple colors.
-
Cytochemical stains depend on the presence of special enzymes, glycogen, lipids, or phosphatases inside the cells.
-
Special stains identify things like iron or reticulin fibers.
Routine Stains
These are the first stains used for bone marrow smears.
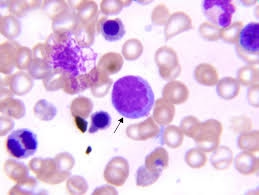
Romanowsky Stains
-
Most common: Leishman, Wright, Giemsa, May–Grünwald–Giemsa (MGG).
-
Principle: Mixture of eosin and methylene blue gives multi-color staining.
-
Results:
-
Red cells → pink-orange
-
Nuclei → purple-blue
-
Neutrophil granules → lilac
-
Basophil granules → deep blue
-
Platelets → violet
-
Procedure (example – Leishman stain):
-
Air-dry smear.
-
Cover with Leishman stain for 2–3 min (fixation).
-
Add equal volume of buffered water for 8–10 min.
-
Wash, air-dry, and examine.
Use: Best for overall morphology.
Cytochemical Stains
These stains help to classify leukemias and confirm cell lineage.
1. Myeloperoxidase (MPO)
-
Detects enzyme in myeloid cells.
-
Positive in AML, negative in ALL.
-
Brown-black granules in cytoplasm.
2. Sudan Black B (SBB)
-
Stains lipids in myeloid granules.
-
Same use as MPO.
-
AML positive, ALL negative.
3. Periodic Acid–Schiff (PAS)
-
Stains glycogen → magenta color.
-
Positive in lymphoblasts in ALL.
-
Also positive in erythroid precursors in erythroleukemia.
4. Esterases
-
Specific esterase (CAE): stains neutrophils.
-
Nonspecific esterase (NSE): stains monocytes, inhibited by sodium fluoride.
-
Use: AML-M4 (myelomonocytic) shows both.
5. Acid Phosphatase
-
Present in many cells.
-
T-ALL cells show focal positivity.
6. Tartrate Resistant Acid Phosphatase (TRAP)
-
Enzyme activity not destroyed by tartrate.
-
Positive in Hairy Cell Leukemia.
7. Alkaline Phosphatase (LAP)
-
Used in neutrophils.
-
High LAP score → leukemoid reaction.
-
Low LAP score → chronic myeloid leukemia (CML).
Special Stains
Iron Stain (Prussian Blue)
-
Detects iron as blue deposits.
-
Uses:
-
Check marrow iron stores.
-
Diagnose iron deficiency anemia (no iron).
-
Detect ring sideroblasts in sideroblastic anemia/MDS.
-
Reticulin Stain
-
Shows reticulin fibers.
-
Used to detect fibrosis in marrow (myelofibrosis, post-chemotherapy).
Microbial Stains
-
Ziehl–Neelsen: TB bacilli.
-
PAS or GMS: Fungal organisms, Leishmania.
Immunostaining and Modern Methods
-
Immunocytochemistry (ICC): Uses antibodies tagged with color.
-
Immunohistochemistry (IHC): Similar, done on biopsy sections.
-
Examples:
-
Myeloid markers: CD13, CD33, CD117.
-
B-cell markers: CD19, CD20, CD79a.
-
T-cell markers: CD3, CD7.
-
Stem cell/blast marker: CD34.
-
Importance: More accurate than cytochemistry for diagnosing leukemias.
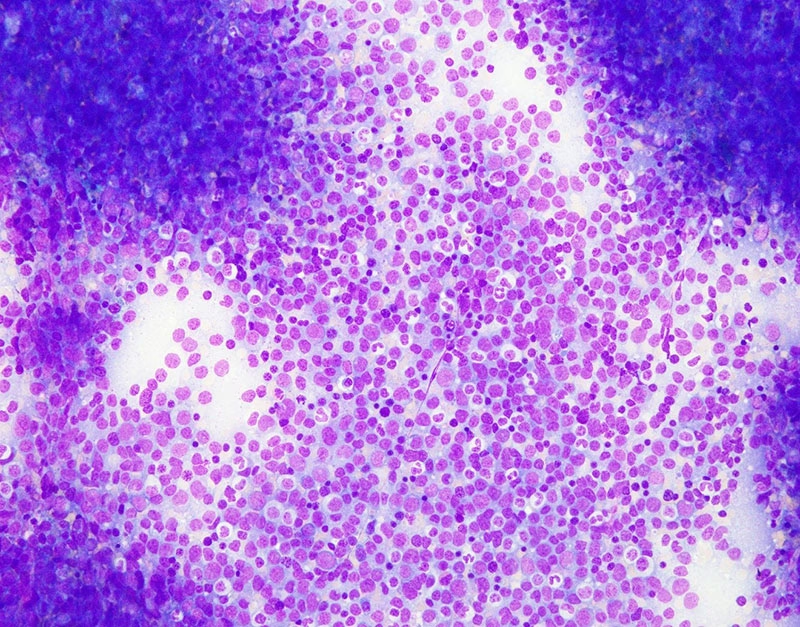
Reading a Stained Smear
After staining, we look for:
-
Cellularity: Rich, normal, or poor.
-
M:E ratio: Normal 2–4:1.
-
Blasts: >20% = acute leukemia.
-
Maturation: Normal or blocked.
-
Iron stores: Normal, increased, or absent.
-
Abnormal cells: Lymphoma cells, plasma cells, metastatic cancer.
-
Fibrosis or parasites.
Clinical Applications
-
Anemias:
-
Iron deficiency → no iron in Prussian blue stain.
-
Sideroblastic anemia → ring sideroblasts.
-
Megaloblastic anemia → large abnormal precursors.
-
-
Leukemias:
-
AML → MPO and SBB positive.
-
ALL → PAS positive.
-
Myelomonocytic leukemia → dual esterase positivity.
-
Hairy cell leukemia → TRAP positive.
-
-
Myeloproliferative disorders:
-
Reticulin stain shows fibrosis.
-
LAP score differentiates CML from leukemoid reaction.
-
-
Infections:
-
Leishmania, Histoplasma, TB, fungi visible on special stains.
-
-
Metastasis:
-
Tumor cells may be seen, confirmed by immunostains.
-
Limitations
-
Romanowsky stains show morphology but not lineage in difficult cases.
-
Cytochemistry sometimes overlaps (MPO-negative AML).
-
Some stains lose activity if smears are old.
-
Technical errors affect results.
-
Immunostains and flow cytometry are better but expensive.
Recent Advances
-
Flow cytometry: Uses fluorescent antibodies, very accurate.
-
Molecular methods (PCR, FISH, NGS): Find gene mutations.
-
Digital imaging: Improves smear analysis.
-
Today, routine stains + immunostains + molecular tests = best diagnosis.