Introduction
- The bone marrow is the central organ of blood formation (hematopoiesis).
- It produces red blood cells (RBCs), white blood cells (WBCs), and platelets that circulate in the peripheral blood.
- Because many blood disorders originate in or involve the bone marrow, direct study of the marrow is essential in hematology, oncology, and pathology.
Two standard techniques exist to obtain bone marrow samples:
-
Bone marrow aspiration – removes liquid marrow, useful for cytology (individual cells).
-
Bone marrow trephine biopsy – removes a solid cylindrical core of marrow and bone, useful for histology (architecture, fibrosis, infiltration).
Anatomy of Bone Marrow
-
Red marrow: active hematopoietic tissue, rich in stem cells, progenitors, and blood cells. Found mainly in flat bones (pelvis, sternum, ribs, vertebrae) and the ends of long bones in adults.
-
Yellow marrow: fatty, inactive marrow, more common in long bones of adults.
-
Vascular supply: Sinusoids allow rapid release of mature blood cells into circulation.
-
Normal cellularity: Roughly estimated as 100 – age ± 10% (e.g., a 40-year-old should have ~60% cellular marrow).
Indications of Trephine Biopsy
Trephine biopsy is ordered when aspiration alone is inadequate or additional information is needed. Major indications include:
-
Unexplained cytopenias: anemia, leukopenia, thrombocytopenia, or pancytopenia.
-
Bone marrow failure syndromes: aplastic anemia, myelodysplastic syndromes.
-
Fibrotic marrow: myelofibrosis or marrow infiltration where aspiration is often a “dry tap.”
-
Leukemia diagnosis and follow-up: to assess blast infiltration, remission, and relapse.
-
Staging of malignancies: lymphoma, multiple myeloma, and solid tumors (breast, prostate, neuroblastoma) to detect marrow involvement.
-
Infections involving marrow: tuberculosis, leishmaniasis, histoplasmosis, HIV.
-
Bone marrow cellularity studies: hypoplastic vs hypercellular states.
-
Monitoring post-treatment: after chemotherapy, stem cell transplantation, or immunosuppressive therapy.
-
Unexplained fever or systemic symptoms: to exclude infiltrative or infectious diseases.
Contraindications
Trephine biopsy is usually safe, but certain conditions may require caution:
-
Absolute contraindications:
-
Severe bleeding disorders (e.g., hemophilia) without correction.
-
Severe infection at biopsy site.
-
-
Relative contraindications:
-
Severe thrombocytopenia (<20,000/µL) – risk of bleeding (may transfuse platelets first).
-
Patients with uncontrolled anticoagulation therapy.
-
Severe osteoporosis or bone fragility (risk of fracture).
-
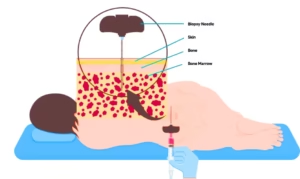
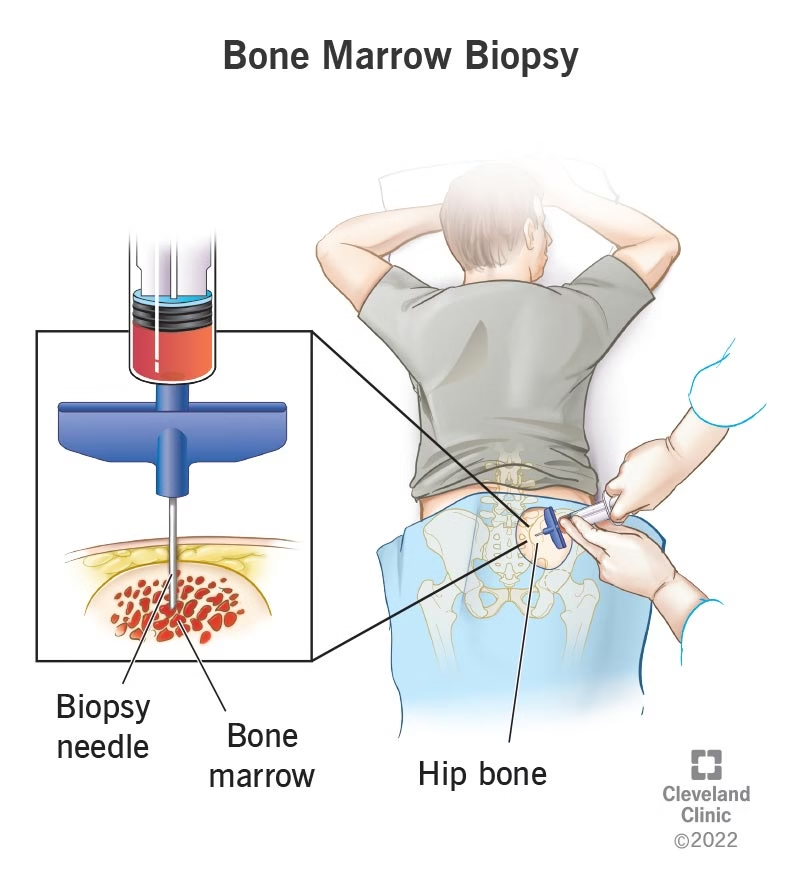
Site of Biopsy
The choice of site is important for both safety and diagnostic yield.
-
Posterior superior iliac crest
-
Most common site in adults and children.
-
Safe, away from major vessels and nerves.
-
Provides adequate sample size.
-
-
Anterior iliac crest
-
Alternative when patient cannot be turned (e.g., critically ill).
-
-
Sternum
-
Used only for aspiration, not trephine, due to risk of injury to heart and great vessels.
-
-
Other sites (rarely used): Tibia (in infants <1 year), vertebrae, or ribs in special circumstances.
Equipment Needed
-
Personal protective equipment (PPE): sterile gloves, gown, mask.
-
Antiseptic solution: povidone-iodine, chlorhexidine.
-
Sterile drapes.
-
Local anesthetic: 1–2% lignocaine.
-
Scalpel blade: for skin nick.
-
Trephine biopsy needle: e.g., Jamshidi needle (most widely used).
-
Syringe (10–20 mL): for aspiration if combined.
-
Specimen container: 10% neutral buffered formalin for biopsy core.
-
Gauze pads and adhesive bandage.
Pre-procedure Preparation
-
Informed consent: Explain purpose, risks, and benefits.
-
History and labs: Check platelet count, coagulation profile, drug history (anticoagulants, aspirin).
-
Positioning:
-
For posterior iliac crest: patient lies on side (lateral decubitus) or prone (face down).
-
For anterior crest: patient lies supine.
-
-
Sedation/analgesia: Local anesthesia is usually enough; mild sedation for children or anxious patients.
Trephine Biopsy Technique
Step 1: Skin preparation
-
Clean the biopsy site with antiseptic solution.
-
Drape with sterile cloth.
Step 2: Local anesthesia
-
Infiltrate skin, subcutaneous tissue, and periosteum with lignocaine.
-
Ensure adequate pain relief before proceeding.
Step 3: Skin incision
-
Make a small skin nick (2–3 mm) with a scalpel to ease needle entry.
Step 4: Needle insertion
-
Insert the Jamshidi trephine needle perpendicular to the iliac crest.
-
Apply firm pressure with a rotating, drilling motion until cortex is penetrated.
-
The operator feels a “give way” when entering the marrow cavity.
Step 5: Advance into marrow
-
Advance needle 1–2 cm into marrow cavity.
-
Continue rotation to cut a cylindrical core of bone + marrow.
Step 6: Core removal
-
Withdraw needle with gentle twisting.
-
Use stylet or probe to push specimen out.
-
Length of specimen: ideally 1–2 cm, intact, not fragmented.
Step 7: Aftercare
-
Apply firm pressure to site for several minutes.
-
Apply sterile dressing.
-
Ask patient to lie on back for 10–15 minutes to reduce bleeding risk.
Handling and Processing of Specimen
-
Place biopsy core immediately into 10% formalin.
-
Do not crush or squeeze specimen.
-
Send to pathology laboratory.
-
Processing: decalcification (to soften bone), embedding in paraffin, sectioning, and staining.
Stains used:
-
Hematoxylin and eosin (H&E).
-
Reticulin stain (to assess fibrosis).
-
Immunohistochemistry (for lymphomas, leukemias).
-
Special stains for infections (AFB, PAS, GMS).
What Can Be Seen in Trephine Biopsy?
-
Cellularity: Ratio of hematopoietic tissue to fat.
-
Hypercellular: leukemia, myeloproliferative disorders.
-
Hypocellular: aplastic anemia.
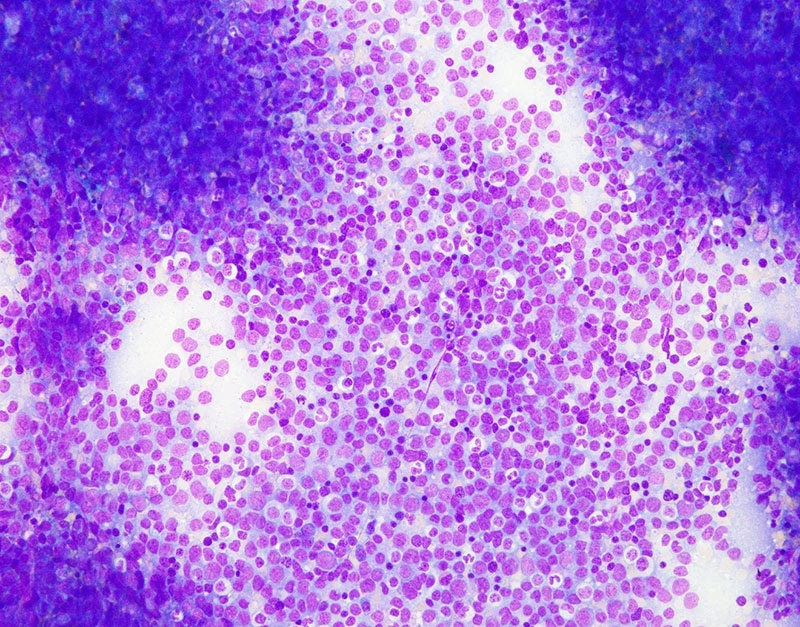
-
-
Distribution of cells:
-
Erythroid, myeloid, and megakaryocytes.
-
Abnormal clusters (e.g., blasts, plasma cells, lymphoma infiltration).
-
-
Fibrosis: Graded using reticulin stain. Seen in myelofibrosis, CML, metastatic tumors.
-
Granulomas: Suggest infections (TB, sarcoidosis).
-
Metastasis: Carcinomas, neuroblastoma, etc.
-
Other features: Necrosis, storage diseases (e.g., Gaucher cells).
Advantages of Trephine Biopsy
-
Provides marrow architecture (aspiration gives single cells only).
-
Useful in “dry tap” cases.
-
Shows fibrosis, infiltration, and granulomas clearly.
-
Detects focal lesions missed in aspiration.
-
Better for estimating overall cellularity.
-
Allows immunohistochemistry and molecular tests.
Limitations
-
More painful than aspiration.
-
Requires special needle and training.
-
Takes longer processing time (due to decalcification).
-
Sample may be inadequate or crushed if technique is poor.
Complications
Though rare, possible complications include:
-
Pain during or after procedure.
-
Local bleeding or hematoma.
-
Infection at site.
-
Rarely: fracture of iliac crest, sciatic nerve injury.
-
Vasovagal syncope in anxious patients.
Prevention: correct coagulopathy, use aseptic technique, ensure proper local anesthesia.
Recent Advances
-
Improved needles: Jamshidi and Klima needles with better core retrieval.
-
Image-guided biopsies: CT or ultrasound for difficult cases.
-
Automated biopsy devices: faster and less painful.
-
Digital pathology and immunohistochemistry: better classification of leukemias/lymphomas.
-
Flow cytometry and molecular tests now often performed on biopsy material.