Introduction
- Trichomonas vaginalis is a flagellated protozoan parasite and the causative agent of trichomoniasis, a common sexually transmitted infection (STI).
- It is the only protozoan known to infect the human urogenital tract and predominantly affects the vagina in females and the urethra or prostate in males.
- Trichomoniasis is characterized by vaginal discharge, irritation, and itching in women, while men are often asymptomatic carriers.
- Despite being treatable, trichomoniasis has significant public health implications due to its association with preterm delivery, low birth weight, and an increased risk of HIV transmission.
Geographical Distribution
Trichomonas vaginalis is distributed worldwide, with the highest prevalence in:
-
- Low- and middle-income countries, particularly in sub-Saharan Africa, Southeast Asia, and Latin America.
- High-risk populations, such as sexually active individuals, those with multiple sexual partners, and people with inadequate access to healthcare or STI prevention measures.
An estimated 156 million new cases of trichomoniasis occur annually, making it one of the most prevalent non-viral STIs globally, according to the World Health Organization (WHO).
Habitat
-
- In females: T. vaginalis resides in the vagina, cervix, and occasionally the urethra or bladder.
- In males: It infects the urethra, prostate gland, or seminal vesicles.
- The parasite thrives in an anaerobic environment, with an optimal pH of 5–6.
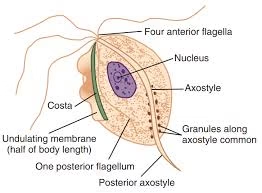
Morphology
Trichomonas vaginalis exists only as a trophozoite; it does not form cysts.
-
- Trophozoite:
- Shape: Pear-shaped or ovoid.
- Size: 7–30 µm in length and 5–12 µm in width.
- Structure:
- A single nucleus is located at the broader end.
- Four anterior flagella and one posterior flagellum are attached to an undulating membrane, providing motility.
- Axostyle: A rod-like structure that protrudes from the posterior end, aiding in attachment to host tissues.
- Hydrogenosomes: Organelles responsible for energy production in anaerobic conditions.
- Trophozoite:
Life Cycle
-
- vaginalis has a direct life cycle involving a single host (humans).
-
- Transmission:
- The trophozoite is transmitted during sexual contact.
- Colonization:
- In females, it adheres to the vaginal epithelium; in males, it infects the urethra or prostate.
- The parasite multiplies by binary fission in anaerobic conditions.
- Survival outside the host:
- The trophozoite can survive for a few hours in moist environments, but its transmission occurs almost exclusively through direct contact.
- Transmission:
Mode of Transmission
- Sexual transmission:
- The primary mode of transmission is through unprotected sexual intercourse (vaginal, anal, or oral).
- Non-sexual transmission (rare):
- Through contaminated objects (e.g., towels, wet surfaces, or medical instruments) due to the parasite’s ability to survive briefly in moist environments.
- Vertical transmission from an infected mother to a newborn during delivery has been reported.
Incubation Time
The incubation period for trichomoniasis is typically 4 to 28 days, although some cases may remain asymptomatic for longer periods.
Pathogenesis
The pathogenicity of T. vaginalis is mediated by its ability to adhere to host epithelial cells, induce inflammation, and produce cytotoxic effects.
-
- Adhesion and colonization:
- The parasite adheres to vaginal or urethral epithelial cells via surface adhesins and proteolytic enzymes.
- Cytotoxicity:
- It damages epithelial cells, causing tissue inflammation and increased vaginal discharge.
- The axostyle mechanically irritates host tissues, contributing to discomfort.
- Immune response:
- The infection triggers an immune response, resulting in leukocyte infiltration and elevated cytokine levels.
- Adhesion and colonization:
Clinical Manifestations:
- In females:
- Vaginal discharge (frothy, yellow-green, and malodorous).
- Vulvovaginal irritation, itching, dysuria, and dyspareunia.
- “Strawberry cervix” (punctate hemorrhages on the cervix).
- In males:
- Often asymptomatic but may present with urethritis, prostatitis, or dysuria.
Laboratory Diagnosis
- Complete blood count
- Microscopy:
- Wet mount preparation of vaginal or urethral discharge reveals motile trophozoites.
- Sensitivity: 50–60%.
- Culture:
- Involves incubating the specimen in specific media (e.g., Diamond’s medium).
- Sensitivity: 75–95%.
- Antigen detection:
- Rapid immunochromatographic tests detect T. vaginalis-specific antigens.
- Nucleic acid amplification tests (NAATs):
- Highly sensitive and specific molecular methods (e.g., PCR) to detect T. vaginalis DNA.
- Point-of-care testing:
- Affordable and fast tests (e.g., OSOM Trichomonas Rapid Test).
Treatment
- First-line therapy:
- Metronidazole (2 g single dose or 500 mg twice daily for 7 days).
- Tinidazole (2 g single dose).
- Alternative approaches:
- Higher doses or prolonged regimens of metronidazole or tinidazole may be required for resistant cases.
- Partner treatment:
- Both sexual partners must be treated simultaneously to prevent reinfection.
- Special considerations:
- Trichomoniasis during pregnancy requires careful management to reduce adverse outcomes, such as preterm labor.
Prevention
- Safe sexual practices:
- Use of condoms to reduce the risk of transmission.
- Limiting the number of sexual partners.
- Regular screening:
- For sexually active individuals, especially those at high risk for STIs.
- Treatment of asymptomatic carriers:
- Screening and treating asymptomatic male partners can reduce reinfection rates.
- Public health education:
- Awareness campaigns on the importance of STI prevention and early treatment.