Introduction
-
Urinary system consists of:
-
A pair of kidneys
-
A pair of ureters
-
Urinary bladder
-
Urethra
-
-
Kidneys produce urine.
-
Urine is conveyed by ureters to the urinary bladder.
-
Urinary bladder stores urine temporarily.
-
Urine is expelled through the urethra during micturition.
Kidney
General Features
-
Each kidney is a large bean-shaped organ situated in the posterior abdominal wall behind the peritoneum.
-
It measures:
-
Length: 7.5 cm
-
Breadth: 5 cm
-
Thickness: 2.5 cm
-
-
The medial concave border has a hilum, through which renal vessels and nerves pass.
Functions of Kidney
The chemical composition of urine reflects the important functions performed by the kidney:
-
Controls water and electrolyte balance in the body
-
Maintains acid–base balance
-
Excretes toxic metabolic waste products (nitrogen, urea, and creatinine)
-
Maintains blood pressure by the renin–angiotensin–aldosterone mechanism
-
Stimulates RBC production in bone marrow through erythropoietin
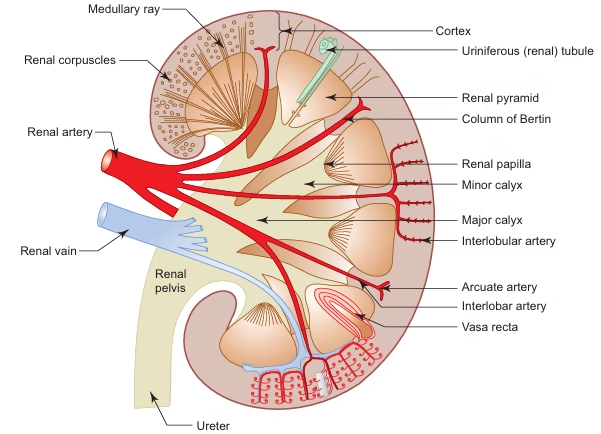
Macroscopic Features
A vertical section through the kidney reveals its gross internal features:
-
The hilum leads to a space called the renal sinus, which contains:
-
Branches of renal vessels and nerves
-
Pelvis of the ureter
-
Major calyces (2–3)
-
Minor calyces (8–12)
-
-
The substance of the kidney is divided into:
-
An outer dark granular (reddish-brown) zone called the cortex
-
An inner pale striated zone called the medulla
-
Medulla
-
The medulla is formed by 8–12 renal pyramids.
-
The bases of the pyramids face the cortex.
-
The apices (renal papillae) are directed toward the renal sinus.
-
Each renal papilla is cupped by a minor calyx.
-
The tip of each papilla is pierced by many papillary ducts (ducts of Bellini) opening into the minor calyx.
Cortex
-
From the base of the pyramids, medullary tissue extends into the cortex as medullary rays.
-
Cortical tissue extends between adjacent pyramids as the renal columns of Bertin.
Microscopic structure of kidney
-
Kidney is composed of numerous uriniferous (renal) tubules.
-
Tubules are embedded in a vascular interstitium.
-
Each uriniferous tubule has two parts:
-
Nephron – produces urine.
-
Collecting tubule – concentrates urine.
-
Uriniferous tubule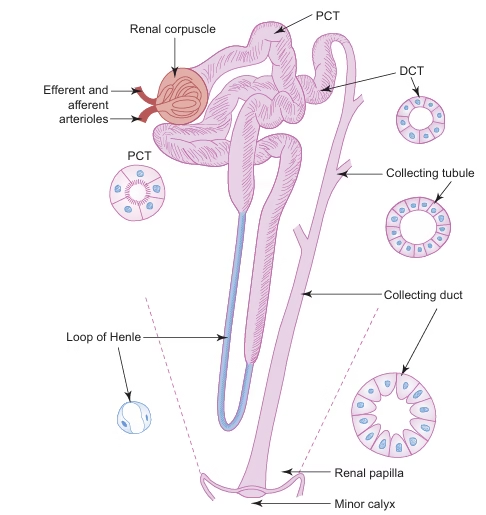
-
Nephron:
-
Derived from metanephric blastema.
-
Concerned with urine formation.
-
-
Collecting tubule:
-
Derived from ureteric bud of mesonephric duct.
-
Responsible for urine concentration (hypertonicity).
-
Nephron
-
Structural and functional unit of kidney.
-
Number: 1–4 million per kidney.
-
Parts:
-
Renal corpuscle.
-
Proximal convoluted tubule (pct).
-
Loop of henle.
-
Distal convoluted tubule (dct).
-
Types of nephrons
-
Cortical nephrons:
-
Located in cortex.
-
Have short loops of henle.
-
Extend up to outer medulla.
-
-
Juxtamedullary nephrons:
-
Located at corticomedullary junction.
-
Have long loops of henle with vasa recta.
-
Create hypertonic medulla.
-
Essential for formation of concentrated urine.
-
Renal corpuscle (malpighian corpuscle)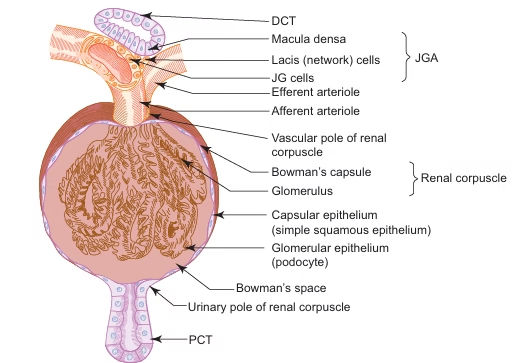
-
Site of blood filtration.
-
Located in cortex.
-
Diameter: approximately 200 µm.
-
Components:
-
Bowman’s capsule.
-
Glomerulus.
-
Bowman’s capsule
-
Blind, cup-shaped end of nephron.
-
Formed by invagination of glomerulus.
-
Consists of two layers:
-
Parietal layer:
-
Lined by simple squamous epithelium.
-
Continuous with pct at urinary pole.
-
-
Visceral layer:
-
Composed of podocytes.
-
-
-
Space between layers:
-
Bowman’s (urinary) space.
-
-
Poles:
-
Vascular pole – entry and exit of arterioles.
-
Urinary pole – origin of pct.
-
Glomerulus
-
Tuft of anastomosing capillaries.
-
Supplied by afferent arteriole (wider).
-
Drained by efferent arteriole (narrower).
-
Pressure gradient produces filtration.
-
Capillaries lined by fenestrated endothelium.
-
Supported by mesangial cells with contractile and phagocytic functions.
-
Nuclei seen belong to endothelial cells, mesangial cells, and podocytes.
Podocytes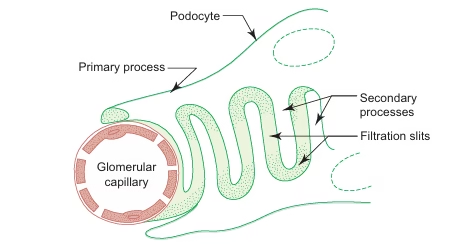
-
Specialized epithelial cells of visceral layer.
-
Possess primary processes.
-
Primary processes give rise to secondary foot processes (pedicels).
-
Pedicels interdigitate forming filtration slits (~25 nm).
-
Filtration slits are bridged by slit membrane.
-
Cell bodies and primary processes do not touch the basement membrane.
Glomerular basement membrane
-
Thickness: approximately 100 nm.
-
Formed by fused basal laminae of endothelium and podocytes.
-
Acts as a selective filtration barrier.
Glomerular filtration barrier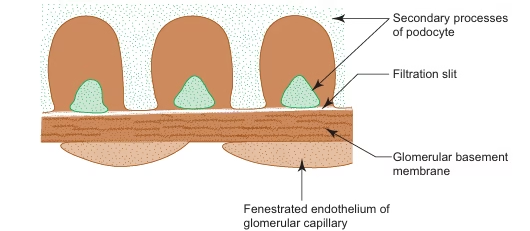
Consists of three layers:
-
Fenestrated endothelium – prevents passage of blood cells.
-
Glomerular basement membrane – blocks particles >10 nm and negatively charged proteins.
-
Filtration slits and slit membrane – final filtration barrier.
Proximal convoluted tubule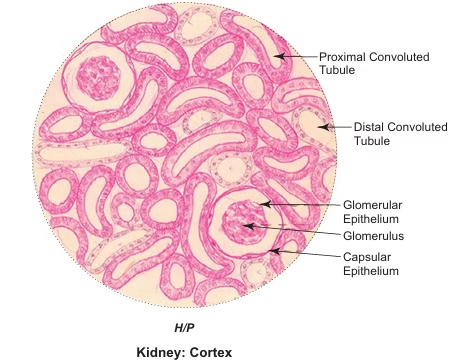
-
Proximal convoluted tubule (pct) starts at the urinary pole of the renal corpuscle.
-
It is longer and more convoluted than distal convoluted tubule.
-
It forms the bulk of the renal cortex.
-
It is lined by simple cuboidal epithelium.
-
Luminal surface has microvilli forming a brush border.
-
Basal surface shows striations due to:
-
Infoldings of plasma membrane
-
Longitudinally arranged mitochondria
-
-
About 75% of water and electrolytes (sodium, potassium, chloride) are reabsorbed by selective reabsorption.
-
It also secretes certain metabolites, dyes, and drugs.
Loop of henle
-
Loop of henle arises from pct in the cortex.
-
It descends into medulla as descending limb.
-
It turns and ascends as ascending limb.
-
It becomes continuous with dct at corticomedullary junction.
Segments of loop of henle
-
Descending limb:
-
Short thick segment (straight part of pct)
-
Long thin segment
-
-
Ascending limb:
-
Short thin segment
-
Long thick segment (straight part of dct)
-
Histology
-
Thick segments:
-
Lined by cuboidal epithelium
-
Impermeable to water
-
-
Thin segments:
-
Lined by simple squamous epithelium
-
Permeable to water and sodium
-
Functional mechanism
-
Descending limb:
-
Passive removal of water
-
-
Ascending limb:
-
Active transport of sodium and chloride
-
-
Tubular fluid becomes:
-
Hypertonic initially
-
Isotonic later
-
Vascular association
-
Loops of henle are closely related to vasa recta.
-
Vasa recta maintain osmotic gradient of medullary interstitium.
Collecting tubule and collecting duct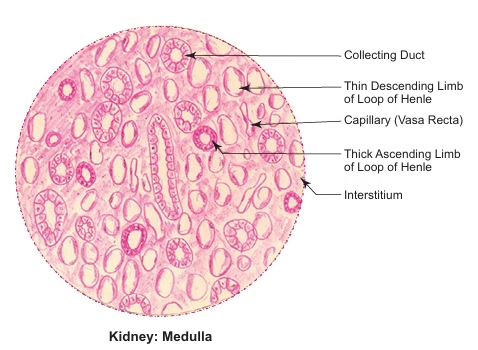
-
Collecting tubule begins in the medullary ray.
-
It is a continuation of distal convoluted tubule.
-
On entering the medulla, several collecting tubules join together.
-
They form a larger duct called duct of bellini or papillary duct.
-
Papillary ducts open at the apex of renal pyramid (renal papilla).
Histology
-
Collecting tubules:
-
Lined by simple cuboidal epithelium
-
Cells have distinct boundaries
-
Cytoplasm is clear and pale
-
-
Collecting ducts (papillary ducts):
-
Larger and wider
-
Lined by tall columnar epithelium
-
Cytoplasm is pale-staining
-
Ureter
General features
-
Ureters are muscular tubes.
-
They conduct urine from renal pelvis to urinary bladder.
-
Transport of urine occurs by peristaltic contractions.
-
Peristalsis is produced by smooth muscle in the ureteric wall.
Structure of ureter
-
Wall of ureter is composed of three coats:
-
Mucosa
-
Muscle coat
-
Adventitia
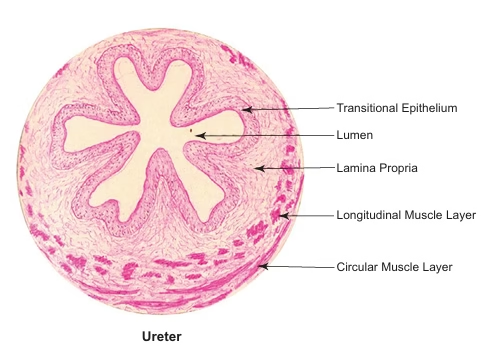
-
Mucosa
-
Lined by transitional epithelium.
-
Supported by lamina propria rich in elastic fibers.
-
Mucosa forms longitudinal folds.
-
Folds give a star-shaped lumen in cross section.
Muscle coat
-
Composed of smooth muscle fibers.
-
Upper two-thirds of ureter have two layers:
-
Inner longitudinal layer
-
Outer circular layer
-
-
Lower one-third of ureter has three layers:
-
Inner longitudinal layer
-
Middle circular layer
-
Outer longitudinal layer
-
Adventitia
-
Outermost coat of ureter.
-
Made of loose connective tissue.
-
Contains blood vessels, lymphatics, and nerves.
Urinary bladder
General features
-
Urinary bladder is a muscular sac.
-
It temporarily stores urine.
-
Urine is expelled through urethra during micturition.
-
Empty bladder lies in pelvis behind pubic symphysis.
-
Shape of empty bladder is four-sided pyramidal.
-
Normal capacity is about 200–300 ml.
Structure of urinary bladder
-
Wall of urinary bladder has three coats:
-
Mucosa
-
Muscle coat
-
Adventitia / serosa
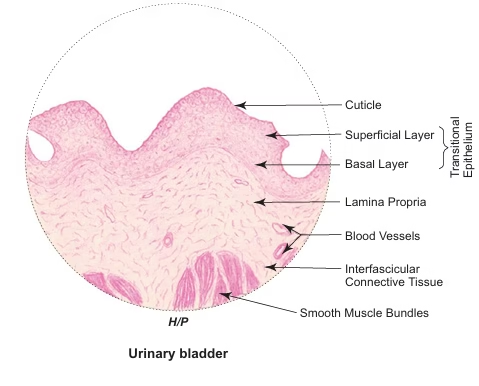
-
Mucosa
-
Lined by transitional epithelium (urothelium).
-
Supported by lamina propria.
-
Urothelium is present only in urinary system.
-
Lines passages from minor calyx to upper urethra.
-
Specially adapted for stretching without damage.
Changes with bladder state
-
When bladder is empty:
-
Mucosa shows folds.
-
Epithelium is thick (5–6 cell layers).
-
Superficial cells are rounded and bulge into lumen.
-
Superficial cells may be binucleate or polyploid.
-
Plasma membrane of superficial cells is thickened.
-
Acts as osmotic barrier against toxic urine.
-
-
When bladder is distended:
-
Mucosal folds disappear.
-
Epithelium becomes thin (3–4 cell layers).
-
Superficial cells become flattened.
-
Muscle coat
-
Made of smooth muscle fibers.
-
Arranged in three ill-defined layers:
-
Inner longitudinal
-
Middle circular
-
Outer longitudinal
-
-
Collectively forms detrusor muscle.
-
Muscle fibers around internal urethral orifice form internal sphincter.
Adventitia / serosa
-
Adventitia is composed of fibroelastic connective tissue.
-
Contains blood vessels, nerves, and lymphatics.
-
Superior surface of bladder is covered by peritoneum.
-
This surface forms serosa instead of adventitia.
MCQs
-
Urinary system consists of
a. Kidneys and ureters only
b. Kidneys, ureters, bladder, and urethra
c. Kidneys and bladder only
d. Bladder and urethra only
Answer: b -
Urine is produced by
a. Ureter
b. Urinary bladder
c. Kidney
d. Urethra
Answer: c -
Temporary storage of urine occurs in
a. Kidney
b. Ureter
c. Urinary bladder
d. Urethra
Answer: c -
Urine is expelled through
a. Ureter
b. Renal pelvis
c. Urethra
d. Minor calyx
Answer: c -
Kidneys are located
a. In pelvic cavity
b. In thoracic cavity
c. On posterior abdominal wall
d. In peritoneal cavity
Answer: c -
Kidneys are situated
a. In front of peritoneum
b. Within peritoneum
c. Behind peritoneum
d. Inside pelvis
Answer: c -
Shape of kidney is
a. Oval
b. Round
c. Bean-shaped
d. Pyramidal
Answer: c -
Length of kidney is approximately
a. 5 cm
b. 7.5 cm
c. 10 cm
d. 12 cm
Answer: b -
Medial border of kidney contains
a. Capsule
b. Papilla
c. Hilum
d. Pyramid
Answer: c -
Renal vessels and nerves pass through
a. Cortex
b. Medulla
c. Hilum
d. Renal pelvis
Answer: c -
Kidney maintains blood pressure by
a. Adh
b. Aldosterone only
c. Renin–angiotensin–aldosterone mechanism
d. Erythropoietin
Answer: c -
Hormone secreted by kidney for rbc production is
a. Renin
b. Aldosterone
c. Adh
d. Erythropoietin
Answer: d -
Outer fibrous covering of kidney is
a. Renal fascia
b. Perinephric fat
c. Fibrous capsule
d. Peritoneum
Answer: c -
Fat surrounding kidney is called
a. Mesenteric fat
b. Perinephric fat
c. Subcutaneous fat
d. Retroperitoneal fat
Answer: b -
Renal fascia is also known as
a. Fascia lata
b. Fascia of gerota
c. Camper’s fascia
d. Scarpa’s fascia
Answer: b -
Renal sinus contains
a. Cortex and medulla
b. Renal pyramids
c. Pelvis and calyces
d. Nephrons
Answer: c -
Number of major calyces is
a. 1
b. 2–3
c. 6–8
d. 10–12
Answer: b -
Number of minor calyces is
a. 2–3
b. 4–6
c. 8–12
d. 15–20
Answer: c -
Outer zone of kidney is
a. Medulla
b. Renal sinus
c. Cortex
d. Pelvis
Answer: c -
Inner pale striated zone of kidney is
a. Cortex
b. Medulla
c. Capsule
d. Hilum
Answer: b -
Renal pyramids are present in
a. Cortex
b. Medulla
c. Pelvis
d. Capsule
Answer: b -
Apex of renal pyramid is called
a. Renal column
b. Medullary ray
c. Renal papilla
d. Minor calyx
Answer: c -
Papillary ducts open into
a. Major calyx
b. Renal pelvis
c. Minor calyx
d. Ureter
Answer: c -
Ducts of bellini open at
a. Cortex
b. Renal sinus
c. Renal papilla
d. Hilum
Answer: c -
Medullary rays extend from
a. Cortex to medulla
b. Medulla to cortex
c. Pelvis to cortex
d. Capsule to cortex
Answer: b -
Renal columns of bertin are
a. Medullary tissue in cortex
b. Cortical tissue between pyramids
c. Collecting ducts
d. Renal tubules
Answer: b -
A renal lobe consists of
a. Pyramid only
b. Cortex only
c. Pyramid with overlying cortex
d. Medullary ray only
Answer: c -
Renal lobule consists of
a. Pyramid and papilla
b. Medullary ray with surrounding cortex
c. Cortex only
d. Medulla only
Answer: b -
Renal artery divides first into
a. Interlobular arteries
b. Arcuate arteries
c. Segmental arteries
d. Afferent arterioles
Answer: c -
Arcuate arteries are located at
a. Hilum
b. Cortex
c. Medulla
d. Corticomedullary junction
Answer: d -
Interlobular arteries give rise to
a. Efferent arterioles
b. Vasa recta
c. Afferent arterioles
d. Renal veins
Answer: c -
Efferent arteriole of cortical nephron forms
a. Vasa recta
b. Peritubular capillary plexus
c. Sinusoids
d. Portal system
Answer: b -
Efferent arteriole of juxtamedullary nephron forms
a. Peritubular plexus
b. Sinusoids
c. Vasa recta
d. Arcuate veins
Answer: c -
Vasa recta help in
a. Filtration
b. Hormone secretion
c. Maintaining medullary osmotic gradient
d. Urine storage
Answer: c -
Renal vein exits kidney through
a. Cortex
b. Medulla
c. Pelvis
d. Hilum
Answer: d -
Structural and functional unit of kidney is
a. Renal corpuscle
b. Collecting duct
c. Nephron
d. Renal pyramid
Answer: c -
Nephron is derived from
a. Ureteric bud
b. Mesonephric duct
c. Metanephric blastema
d. Pronephros
Answer: c -
Collecting tubule is derived from
a. Metanephric blastema
b. Ureteric bud
c. Cloaca
d. Allantois
Answer: b -
Number of nephrons per kidney is
a. 10,000
b. 50,000
c. 1–4 million
d. 10 million
Answer: c -
Cortical nephrons have
a. Long loop of henle
b. Vasa recta
c. Short loop of henle
d. No loop of henle
Answer: c -
Juxtamedullary nephrons are located at
a. Cortex only
b. Medulla only
c. Corticomedullary junction
d. Renal pelvis
Answer: c -
Renal corpuscle is present in
a. Medulla
b. Cortex
c. Pelvis
d. Papilla
Answer: b -
Diameter of renal corpuscle is about
a. 50 µm
b. 100 µm
c. 200 µm
d. 500 µm
Answer: c -
Bowman’s capsule has
a. One layer
b. Two layers
c. Three layers
d. Four layers
Answer: b -
Visceral layer of bowman’s capsule is made of
a. Mesangial cells
b. Endothelial cells
c. Podocytes
d. Fibroblasts
Answer: c -
Filtration slits are formed between
a. Endothelial cells
b. Podocyte pedicels
c. Mesangial cells
d. Basement membrane
Answer: b -
Thickness of glomerular basement membrane is about
a. 25 nm
b. 50 nm
c. 75 nm
d. 100 nm
Answer: d -
Glomerular filtrate is similar to plasma except for
a. Glucose
b. Electrolytes
c. Plasma proteins
d. Water
Answer: c -
Normal urine output per day is approximately
a. 500 ml
b. 1000 ml
c. 1500 ml
d. 3000 ml
Answer: c -
Ureters conduct urine by
a. Gravity
b. Diffusion
c. Peristaltic contraction
d. Osmosis
Answer: c