Introduction
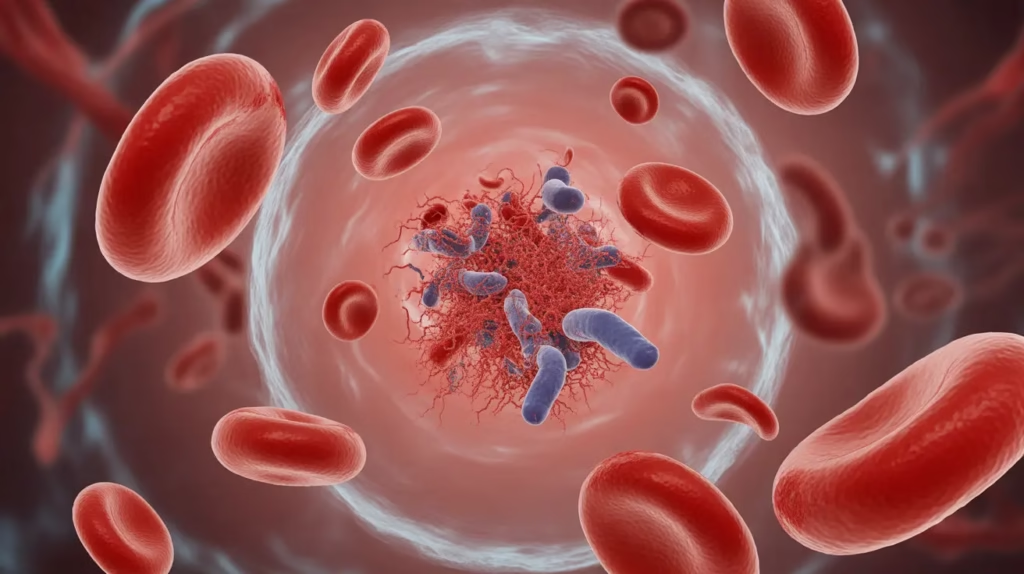
- Blood transfusion is a life-saving therapeutic procedure widely used in medical and surgical practice, but it is not without risk.
- A transfusion reaction refers to any adverse clinical event occurring during or after the transfusion of whole blood or blood components, irrespective of its severity.
- Transfusion reactions may be mild, moderate, or life-threatening, ranging from simple febrile or allergic reactions to severe complications such as acute hemolytic reaction, sepsis, TRALI, and circulatory overload.
- These reactions can occur due to immune-mediated mechanisms (e.g., ABO incompatibility, alloantibody formation) or non-immune causes (e.g., bacterial contamination, volume overload, mechanical hemolysis).
- Based on timing, transfusion reactions are classified into acute reactions (occurring during transfusion or within 24 hours) and delayed reactions (developing days to weeks later).
- Acute hemolytic transfusion reaction, most commonly due to ABO mismatch, is a medical emergency associated with high morbidity and mortality if not promptly recognized and managed.
- Clinical manifestations of transfusion reactions are often non-specific and may mimic other acute conditions such as sepsis, allergic reactions, or cardiac failure, making diagnosis challenging.
- Therefore, immediate clinical assessment combined with systematic laboratory investigation is essential to confirm the diagnosis, identify the underlying cause, and guide appropriate management.
- Laboratory evaluation plays a crucial role in:
- Detecting blood group incompatibility
- Identifying immune or non-immune hemolysis
- Assessing severity and complications such as DIC or renal failure
- Preventing recurrence in future transfusions
- A well-defined transfusion reaction investigation protocol also supports hemovigilance systems, improves transfusion safety, and enhances overall quality of patient care.
Etiology
I. Immune-Mediated Causes
These reactions occur due to antigen–antibody interactions between donor blood components and the recipient.
1. ABO Incompatibility
- Most common and most severe cause of acute hemolytic transfusion reaction
- Occurs due to clerical errors, mislabeling, or incorrect patient identification
- Naturally occurring IgM antibodies activate complement
- Leads to intravascular hemolysis, shock, DIC, and acute renal failure
2. Rh Incompatibility
- Occurs mainly in Rh-negative recipients receiving Rh-positive blood
- Usually causes delayed hemolytic transfusion reactions
- Mediated by IgG antibodies
- Less severe than ABO mismatch but clinically significant
3. Alloantibodies Against Minor Blood Group Antigens
- Antibodies against Kell, Duffy, Kidd, MNS systems
- Develop following previous transfusions or pregnancy
- Responsible for delayed hemolytic transfusion reactions (DHTR)
- Often missed during routine compatibility testing
4. Febrile Non-Hemolytic Transfusion Reaction (FNHTR)
- Caused by:
- Recipient antibodies against donor leukocytes
- Cytokines accumulated during blood storage
- Common with platelet and whole blood transfusions
5. Allergic Reactions
- Due to hypersensitivity to donor plasma proteins
- Range from mild urticaria to severe anaphylaxis
- More common with plasma-rich products
6. Anaphylactic Reaction
- Seen in patients with IgA deficiency
- Caused by anti-IgA antibodies reacting with donor IgA
- Rapid onset with bronchospasm, hypotension, shock
7. Transfusion-Related Acute Lung Injury (TRALI)
- Caused by donor anti-leukocyte or anti-HLA antibodies
- Leads to immune-mediated pulmonary capillary damage
- Results in non-cardiogenic pulmonary edema
II. Non-Immune-Mediated Causes
These reactions are not antibody-mediated and result from physical, chemical, or biological factors.
1. Bacterial Contamination of Blood Products
- Commonly associated with platelets (stored at room temperature)
- Caused by improper collection or storage
- Leads to septic transfusion reaction
- Presents with high fever, hypotension, shock
2. Mechanical Hemolysis
- Caused by:
- Use of small-gauge needles
- Faulty transfusion pumps
- Excessive pressure during transfusion
- Leads to non-immune intravascular hemolysis
3. Thermal Injury
- Transfusion of overheated or improperly warmed blood
- Causes RBC membrane damage and hemolysis
4. Chemical Hemolysis
- Occurs due to contamination with:
- Hypotonic solutions
- Drugs or IV fluids
- Results in RBC destruction
5. Transfusion-Associated Circulatory Overload (TACO)
- Caused by rapid or excessive transfusion volume
- Common in:
- Elderly
- Pediatric patients
- Cardiac or renal failure patients
- Results in cardiogenic pulmonary edema
III. Metabolic and Storage-Related Causes
These occur due to biochemical changes in stored blood.
1. Citrate Toxicity
- Citrate used as anticoagulant binds calcium
- Causes hypocalcemia, especially in massive transfusion
- Leads to paresthesia, tetany, arrhythmias
2. Hyperkalemia
- Potassium leaks from stored RBCs
- Risk increased in massive or rapid transfusions
- Particularly dangerous in neonates and renal failure patients
3. Hypothermia
- Infusion of cold blood products
- Can cause cardiac arrhythmias and coagulopathy
IV. Procedural and Clerical Errors
- Incorrect patient identification
- Wrong labeling of samples
- Errors in blood grouping or crossmatching
- Transfusion of wrong blood component
- Failure to follow transfusion protocols
➡ Most preventable cause of serious transfusion reactions
V. Patient-Related Risk Factors
- Previous transfusions
- History of transfusion reactions
- Pregnancy (alloimmunization)
- IgA deficiency
- Cardiac or renal disease
- Immunocompromised state
Epidemiology
Distribution by Type of Transfusion Reaction
- Febrile Non-Hemolytic Transfusion Reactions (FNHTR)
- Most common transfusion reaction
- Occurs in 0.1–1% of red cell transfusions
- Higher incidence with platelet transfusions
- Frequency reduced significantly by leukoreduction
- Allergic Reactions
- Occur in 1–3% of plasma-containing transfusions
- Mostly mild (urticaria, itching)
- Severe anaphylactic reactions are very rare
- Acute Hemolytic Transfusion Reactions (AHTR)
- Incidence: ~1 in 38,000–70,000 transfusions
- Most commonly caused by ABO incompatibility
- Majority due to clerical or identification errors, not laboratory testing failure
- Delayed Hemolytic Transfusion Reactions (DHTR)
- Under-reported due to delayed onset
- Incidence increases in multiply transfused patients
- Common in patients with hematologic disorders
- Transfusion-Related Acute Lung Injury (TRALI)
- One of the leading causes of transfusion-related mortality
- Incidence: 1 in 5,000–10,000 transfusions
- Risk higher with plasma-rich components
- Reduced by use of male-only plasma donors
- Transfusion-Associated Circulatory Overload (TACO)
- Incidence: 1–8% in high-risk populations
- Now reported as the most common cause of transfusion-related death in many hemovigilance systems
- Frequently underdiagnosed
- Septic (Bacterial) Transfusion Reactions
- Rare but highly fatal
- More common with platelet transfusions due to room-temperature storage
- Estimated incidence: 1 in 100,000–250,000 transfusions
Population-Based Risk Distribution
- Higher risk groups include:
- Elderly patients
- Neonates and pediatric patients
- Patients with cardiac or renal disease
- Immunocompromised individuals
- Patients receiving massive or repeated transfusions
- Gender differences:
- TRALI historically more common with plasma from multiparous female donors
- Risk reduced with revised donor selection policies
Component-Specific Epidemiology
- Platelets:
- Highest rate of transfusion reactions (febrile and septic)
- Plasma:
- Higher risk of allergic reactions and TRALI
- Packed Red Cells:
- Most commonly associated with hemolytic reactions
Geographical and System-Based Factors
- Incidence varies by:
- Transfusion practices
- Hemovigilance reporting systems
- Quality control measures
- Developed countries report higher incidence due to better surveillance, not necessarily higher true rates
Pathophysiology
I. Immune-Mediated Transfusion Reactions
These occur due to antigen–antibody interactions between donor blood components and recipient immune system.
1. Acute Hemolytic Transfusion Reaction (AHTR)
Mechanism:
- Occurs most commonly due to ABO incompatibility
- Recipient has preformed IgM antibodies against donor RBC antigens
- IgM antibodies rapidly activate the complement system
Pathophysiological Events:
- Complement activation → intravascular hemolysis
- Rapid destruction of donor RBCs
- Release of:
- Free hemoglobin
- LDH
- Potassium
- Hemoglobin binds haptoglobin → depletion
- Free hemoglobin filtered by kidneys → hemoglobinuria
- Nitric oxide scavenging → vasoconstriction
- Cytokine release → fever, hypotension
- Severe cases → DIC, acute renal failure, shock
2. Delayed Hemolytic Transfusion Reaction (DHTR)
Mechanism:
- Occurs days to weeks after transfusion
- Due to IgG alloantibodies formed against minor blood group antigens
- Common antigens: Kell, Kidd, Duffy
Pathophysiological Events:
- Antibody-coated RBCs removed by macrophages
- Extravascular hemolysis (spleen and liver)
- Gradual fall in hemoglobin
- Mild jaundice and anemia
- Usually less severe but clinically significant
3. Febrile Non-Hemolytic Transfusion Reaction (FNHTR)
Mechanism:
- Recipient antibodies against donor leukocytes
- Cytokines (IL-1, IL-6, TNF-α) accumulated during blood storage
Pathophysiology:
- Cytokine release causes:
- Fever
- Chills
- Rigors
- No RBC destruction
- Common with platelet transfusions
4. Allergic Transfusion Reaction
Mechanism:
- IgE-mediated hypersensitivity to donor plasma proteins
Pathophysiology:
- Mast cell degranulation
- Histamine release
- Causes:
- Urticaria
- Pruritus
- Flushing
5. Anaphylactic Transfusion Reaction
Mechanism:
- Occurs in IgA-deficient recipients
- Recipient anti-IgA antibodies react with donor IgA
Pathophysiology:
- Massive mediator release
- Vasodilation and bronchoconstriction
- Rapid onset of:
- Hypotension
- Bronchospasm
- Shock
6. Transfusion-Related Acute Lung Injury (TRALI)
Mechanism (Two-Hit Hypothesis):
- First hit: Recipient clinical condition primes pulmonary neutrophils
- Second hit: Donor anti-HLA or anti-neutrophil antibodies activate neutrophils
Pathophysiological Events:
- Neutrophil activation in pulmonary capillaries
- Endothelial damage
- Capillary leak
- Non-cardiogenic pulmonary edema
- Acute hypoxemia within 6 hours
II. Non-Immune-Mediated Transfusion Reactions
These reactions occur without antigen–antibody interactions.
1. Transfusion-Associated Circulatory Overload (TACO)
Mechanism:
- Rapid or excessive transfusion volume
- Compromised cardiac or renal function
Pathophysiology:
- Increased intravascular volume
- Elevated pulmonary capillary pressure
- Cardiogenic pulmonary edema
- Hypertension and respiratory distress
2. Septic Transfusion Reaction
Mechanism:
- Bacterial contamination of blood products
- More common in platelets (room temperature storage)
Pathophysiology:
- Endotoxin release
- Systemic inflammatory response
- Cytokine storm
- Septic shock and multiorgan failure
3. Mechanical Hemolysis
Mechanism:
- Physical damage to RBCs due to:
- Small-bore needles
- Faulty pumps
- Excessive pressure
Pathophysiology:
- RBC membrane rupture
- Non-immune intravascular hemolysis
4. Thermal and Chemical Hemolysis
Thermal Injury:
- Overheating blood damages RBC membranes
Chemical Injury:
- Hypotonic fluids or drug contamination
- Causes RBC lysis
III. Metabolic and Storage-Related Pathophysiology
1. Citrate Toxicity
- Citrate binds calcium
- Leads to hypocalcemia
- Causes paresthesia, tetany, arrhythmias
2. Hyperkalemia
- Potassium leaks from stored RBCs
- Dangerous in neonates and renal failure
3. Hypothermia
- Cold blood infusion
- Causes arrhythmias and coagulopathy
Evaluation of Transfusion Reaction
I. Immediate Clinical Evaluation
- Stop the transfusion immediately at the first suspicion of a reaction
- Maintain IV access with normal saline
- Record:
- Time of onset of symptoms
- Type and volume of blood component transfused
- Vital signs (temperature, BP, pulse, respiratory rate, oxygen saturation)
- Assess for life-threatening features:
- Hypotension or shock
- Respiratory distress
- Chest or back pain
- Hemoglobinuria
- Altered mental status
- Signs of anaphylaxis
II. Bedside and Clerical Evaluation
- Recheck patient identity:
- Wristband
- Blood bag label
- Compatibility tag
- Verify:
- Patient name and ID number
- Blood group and Rh type
- Unit number and expiry date
- Clerical error is the most common cause of fatal transfusion reactions, especially ABO mismatch
III. Sample Collection for Laboratory Evaluation
The following must be sent immediately to the laboratory:
- Patient’s post-transfusion blood sample (EDTA and plain)
- Remaining donor blood unit with tubing
- Patient’s urine sample (if hemolysis suspected)
- Pre-transfusion sample (if available for comparison)
IV. Basic Laboratory Evaluation
1. Repeat ABO and Rh Typing
- Performed on:
- Patient sample
- Donor unit
- Confirms or excludes ABO/Rh mismatch
Interpretation:
- Any discrepancy strongly suggests acute hemolytic transfusion reaction
2. Repeat Crossmatch
- Major crossmatch (recipient serum vs donor RBCs)
Interpretation:
- Incompatible crossmatch → immune incompatibility
- Compatible crossmatch → consider minor antigen mismatch or non-immune causes
3. Direct Antiglobulin Test (DAT / Direct Coombs Test)
- Detects antibodies or complement bound to RBCs
Interpretation:
- Positive DAT → immune-mediated hemolysis
- Negative DAT → non-immune hemolysis or non-hemolytic reaction
4. Visual Inspection for Hemolysis
- Centrifuged plasma examined for color
Findings:
- Pink/red plasma → hemoglobinemia
- Clear plasma → hemolysis unlikely
Urine Examination:
- Red/brown urine with no RBCs → hemoglobinuria
V. Hemolysis Workup
Performed when hemolytic reaction is suspected:
- Hemoglobin & Hematocrit
- Unexpected fall post-transfusion suggests hemolysis
- Serum Bilirubin
- Raised indirect bilirubin → hemolysis
- Lactate Dehydrogenase (LDH)
- Elevated due to RBC destruction
- Serum Haptoglobin
- Low or absent in intravascular hemolysis
- Reticulocyte Count
- Elevated in delayed hemolytic reactions
VI. Evaluation for Complications
1. Renal Function Tests
- Serum creatinine
- Blood urea
- Urine output monitoring
Purpose: Detect acute kidney injury due to hemoglobinuria
2. Coagulation Profile
- PT
- aPTT
- D-dimer
- Fibrinogen
Purpose: Identify disseminated intravascular coagulation (DIC) in severe hemolysis
VII. Evaluation for Infectious (Septic) Transfusion Reaction
Indicated when high fever, chills, or shock is present:
- Blood cultures:
- From patient
- From donor blood unit
- Gram stain of blood product if available
Positive cultures confirm bacterial contamination, a medical emergency
VIII. Evaluation for Pulmonary Transfusion Reactions
1. TRALI Evaluation
- Acute respiratory distress within 6 hours
- Chest X-ray: bilateral pulmonary infiltrates
- Normal cardiac function
- Exclusion of fluid overload
2. TACO Evaluation
- Signs of volume overload
- Raised BP, JVP
- Pulmonary edema on chest X-ray
- Response to diuretics
IX. Immunohematological Evaluation
- Antibody screening and identification
- Detection of alloantibodies against minor blood group antigens
- Comparison with previous transfusion history
X. Documentation and Reporting
- Record all clinical findings and laboratory results
- Report reaction to:
- Blood bank
- Transfusion committee
- Hemovigilance system
- Label patient records clearly for future transfusion precautions
Diagnosis
I. Basis of Diagnosis
Diagnosis is established on the following pillars:
- Temporal relationship between transfusion and onset of symptoms
- Clinical manifestations during or after transfusion
- Laboratory evidence of hemolysis, immune reaction, infection, or overload
- Exclusion of alternative causes (sepsis, cardiac failure, drug reactions)
II. Clinical Diagnostic Criteria
A transfusion reaction should be suspected when any of the following occur during or within hours of transfusion:
- Fever (≥1°C rise)
- Chills or rigors
- Hypotension or shock
- Chest, back, or flank pain
- Dyspnea, hypoxia
- Dark or red urine
- Rash, urticaria, bronchospasm
- Sudden respiratory distress
- Unexplained bleeding or oozing
👉 Early recognition is critical, especially for acute hemolytic reactions.
III. Laboratory Diagnosis (Core Diagnostic Tests)
1. Repeat ABO and Rh Typing
- Confirms or excludes ABO/Rh incompatibility
- Any discrepancy between patient and donor blood groups is diagnostic of mismatched transfusion
2. Direct Antiglobulin Test (DAT / Direct Coombs Test)
Diagnostic Role:
- Detects antibodies or complement attached to RBCs
Interpretation:
- Positive DAT → immune-mediated hemolytic transfusion reaction
- Negative DAT → excludes immune hemolysis but not non-immune causes
3. Evidence of Hemolysis (Diagnostic Panel)
Diagnosis of hemolytic transfusion reaction is supported by:
- Hemoglobinemia (pink/red plasma)
- Hemoglobinuria (dark urine without RBCs)
- ↓ Hemoglobin / Hematocrit
- ↑ Indirect bilirubin
- ↑ LDH
- ↓ Serum haptoglobin
Presence of these findings strongly confirms acute hemolytic transfusion reaction.
4. Crossmatch Re-testing
- Incompatible crossmatch → confirms immune incompatibility
- Compatible crossmatch → suggests minor antigen reaction or non-immune cause
IV. Diagnosis of Specific Transfusion Reactions
1. Acute Hemolytic Transfusion Reaction
Diagnostic Features:
- Onset: During or within hours
- Positive DAT
- Laboratory evidence of intravascular hemolysis
- Often due to ABO mismatch
2. Delayed Hemolytic Transfusion Reaction
Diagnostic Features:
- Onset: Days to weeks after transfusion
- Gradual fall in hemoglobin
- Positive DAT
- Newly detected alloantibodies
3. Febrile Non-Hemolytic Transfusion Reaction
Diagnostic Features:
- Fever and chills only
- No laboratory evidence of hemolysis
- Normal DAT
- Diagnosis of exclusion
4. Allergic Transfusion Reaction
Diagnostic Features:
- Urticaria, itching, flushing
- Normal laboratory tests
- Diagnosis based on clinical presentation
5. Anaphylactic Reaction
Diagnostic Features:
- Sudden hypotension, bronchospasm, shock
- Occurs within minutes
- Often in IgA-deficient patients
- Diagnosis is primarily clinical
6. Septic Transfusion Reaction
Diagnostic Features:
- High fever, hypotension, shock
- Positive blood cultures from:
- Patient
- Donor blood unit
- Diagnosis confirms bacterial contamination
7. TRALI (Transfusion-Related Acute Lung Injury)
Diagnostic Criteria:
- Acute respiratory distress within 6 hours
- Hypoxemia
- Bilateral pulmonary infiltrates on chest X-ray
- Normal cardiac function
- No evidence of fluid overload
8. TACO (Transfusion-Associated Circulatory Overload)
Diagnostic Criteria:
- Signs of volume overload
- Hypertension, raised JVP
- Pulmonary edema on chest X-ray
- Improves with diuretics
- Evidence of cardiac dysfunction
V. Differential Diagnosis
- Sepsis unrelated to transfusion
- Acute cardiac failure
- Drug-induced reactions
- Pulmonary embolism
- Acute respiratory distress syndrome (non-transfusion related)
VI. Diagnostic Documentation
- Diagnosis must be:
- Clearly documented in patient records
- Communicated to blood bank
- Reported under hemovigilance programs
- Patient should be labeled as “history of transfusion reaction” for future transfusions
Complications
I. Hematological Complications
1. Acute Intravascular Hemolysis
- Massive destruction of donor red blood cells
- Commonly due to ABO incompatibility
- Leads to:
- Hemoglobinemia
- Hemoglobinuria
- Severe anemia
- Can rapidly progress to shock and multiorgan failure
2. Delayed Hemolytic Anemia
- Occurs days to weeks after transfusion
- Due to alloantibody-mediated destruction of transfused RBCs
- Causes:
- Gradual fall in hemoglobin
- Jaundice
- Reticulocytosis
- Often underdiagnosed
3. Disseminated Intravascular Coagulation (DIC)
- Triggered by severe hemolysis or septic transfusion reactions
- Widespread activation of coagulation cascade
- Leads to:
- Consumption of clotting factors
- Bleeding from multiple sites
- Microvascular thrombosis
II. Renal Complications
1. Acute Kidney Injury (AKI)
- Caused by:
- Hemoglobin-induced tubular injury
- Hypotension and renal ischemia
- Common in acute hemolytic reactions
- May progress to:
- Oliguria or anuria
- Need for dialysis
III. Cardiovascular Complications
1. Shock
- Can be:
- Hypovolemic
- Septic
- Anaphylactic
- Results from massive cytokine release or hemolysis
- Presents with hypotension and poor tissue perfusion
2. Transfusion-Associated Circulatory Overload (TACO)
- Causes acute cardiac decompensation
- Leads to:
- Pulmonary edema
- Hypertension
- Heart failure exacerbation
- Common in elderly and pediatric patients
IV. Pulmonary Complications
1. Transfusion-Related Acute Lung Injury (TRALI)
- One of the leading causes of transfusion-related mortality
- Causes:
- Acute hypoxemic respiratory failure
- Non-cardiogenic pulmonary edema
- Often requires:
- Mechanical ventilation
- ICU admission
2. Acute Respiratory Failure
- Can occur secondary to:
- TRALI
- TACO
- Anaphylaxis
- May progress to acute respiratory distress syndrome (ARDS)
V. Infectious Complications
1. Septic Shock
- Due to bacterial contamination of blood products
- Rapid onset with:
- High fever
- Hypotension
- Multiorgan dysfunction
- High mortality if not treated promptly
2. Secondary Infections
- Immunomodulation following transfusion
- Increased susceptibility to nosocomial infections
VI. Metabolic and Electrolyte Complications
1. Hyperkalemia
- Due to potassium leakage from stored RBCs
- Can cause:
- Cardiac arrhythmias
- Cardiac arrest
2. Hypocalcemia
- Caused by citrate toxicity in massive transfusions
- Leads to:
- Tetany
- Arrhythmias
- Hypotension
3. Hypothermia
- Rapid infusion of cold blood products
- Results in:
- Cardiac arrhythmias
- Coagulopathy
VII. Immunological Complications
1. Alloimmunization
- Development of antibodies against RBC antigens
- Complicates future transfusions
- Increases risk of delayed hemolytic reactions
2. Anaphylaxis
- Severe, rapid hypersensitivity reaction
- Can cause:
- Airway obstruction
- Circulatory collapse
- Potentially fatal without immediate treatment
VIII. Mortality
- Severe transfusion reactions can be fatal
- Leading causes of transfusion-related death include:
- TRALI
- TACO
- Acute hemolytic transfusion reactions
- Septic reactions
MCQs
1. A transfusion reaction is best defined as:
A. Any infection transmitted by blood
B. Any adverse event during or after transfusion
C. Only immune-mediated complications
D. Only fatal reactions
✅ Answer: B
2. The most common cause of acute hemolytic transfusion reaction is:
A. Rh incompatibility
B. Minor blood group mismatch
C. ABO incompatibility
D. Leukocyte antibodies
✅ Answer: C
3. Acute hemolytic transfusion reaction is mainly mediated by:
A. IgG antibodies
B. IgE antibodies
C. IgM antibodies
D. IgA antibodies
✅ Answer: C
4. The primary mechanism of RBC destruction in ABO mismatch is:
A. Extravascular hemolysis
B. Intravascular hemolysis
C. Phagocytosis in spleen
D. Apoptosis
✅ Answer: B
5. Direct Antiglobulin Test (DAT) detects:
A. Free antibodies in serum
B. Antibodies bound to RBCs
C. Complement in plasma
D. Platelet antibodies
✅ Answer: B
6. A positive DAT indicates:
A. Non-immune hemolysis
B. Mechanical hemolysis
C. Immune-mediated hemolysis
D. Thermal injury
✅ Answer: C
7. Which finding is most characteristic of intravascular hemolysis?
A. Increased haptoglobin
B. Hemoglobinuria
C. Splenomegaly
D. Reticulocytopenia
✅ Answer: B
8. The earliest laboratory sign of hemolytic transfusion reaction is:
A. Raised bilirubin
B. Drop in hemoglobin
C. Hemoglobinemia
D. Reticulocytosis
✅ Answer: C
9. Serum haptoglobin levels in acute hemolysis are:
A. Increased
B. Normal
C. Decreased
D. Unchanged
✅ Answer: C
10. Delayed hemolytic transfusion reactions are usually mediated by:
A. IgM antibodies
B. IgG antibodies
C. IgE antibodies
D. IgA antibodies
✅ Answer: B
11. Delayed hemolytic transfusion reaction usually occurs:
A. Within 1 hour
B. Within 6 hours
C. 24–48 hours
D. Days to weeks later
✅ Answer: D
12. Which blood group system is commonly involved in delayed hemolytic reactions?
A. ABO
B. Rh only
C. Kell
D. Lewis
✅ Answer: C
13. Febrile non-hemolytic transfusion reaction is caused by:
A. ABO mismatch
B. Cytokines and leukocyte antibodies
C. Bacterial toxins
D. Plasma proteins
✅ Answer: B
14. FNHTR is most commonly associated with transfusion of:
A. Packed RBCs
B. Plasma
C. Platelets
D. Cryoprecipitate
✅ Answer: C
15. Leukoreduction mainly helps prevent:
A. TRALI
B. FNHTR
C. TACO
D. Anaphylaxis
✅ Answer: B
16. Allergic transfusion reactions are usually caused by:
A. RBC antigens
B. Platelet antigens
C. Plasma proteins
D. Bacterial endotoxins
✅ Answer: C
17. Severe anaphylactic reaction is commonly seen in patients with:
A. Hemophilia
B. Sickle cell disease
C. IgA deficiency
D. Iron deficiency anemia
✅ Answer: C
18. TRALI usually occurs within:
A. 24 hours
B. 12 hours
C. 6 hours
D. 72 hours
✅ Answer: C
19. TRALI is characterized by:
A. Cardiogenic pulmonary edema
B. Non-cardiogenic pulmonary edema
C. Pleural effusion
D. Pneumothorax
✅ Answer: B
20. The main pathogenic mechanism in TRALI is:
A. Volume overload
B. IgE-mediated allergy
C. Neutrophil activation in lungs
D. Hemoglobin toxicity
✅ Answer: C
21. TACO is primarily caused by:
A. Immune reaction
B. Bacterial contamination
C. Rapid volume overload
D. Cytokine release
✅ Answer: C
22. Which patient is at highest risk for TACO?
A. Young healthy adult
B. Trauma patient
C. Elderly with heart failure
D. Blood donor
✅ Answer: C
23. Septic transfusion reactions are most commonly associated with:
A. Whole blood
B. Packed RBCs
C. Platelets
D. Cryoprecipitate
✅ Answer: C
24. Platelets have higher risk of bacterial contamination because they are stored at:
A. −20°C
B. 2–6°C
C. Room temperature
D. 37°C
✅ Answer: C
25. The most important immediate step when transfusion reaction is suspected is:
A. Give antibiotics
B. Continue transfusion slowly
C. Stop transfusion
D. Send blood culture
✅ Answer: C
26. Pink-colored plasma after centrifugation indicates:
A. Lipemia
B. Icterus
C. Hemolysis
D. Infection
✅ Answer: C
27. Which laboratory test best confirms immune hemolysis?
A. ESR
B. DAT
C. PT
D. Bleeding time
✅ Answer: B
28. Which complication is most feared in acute hemolytic transfusion reaction?
A. Hypertension
B. Acute kidney injury
C. Hypoglycemia
D. Hypercalcemia
✅ Answer: B
29. Hemoglobinuria can lead to renal failure by causing:
A. Glomerulonephritis
B. Tubular obstruction
C. Immune complex deposition
D. Renal stones
✅ Answer: B
30. DIC in transfusion reaction occurs due to:
A. Platelet deficiency
B. Excess anticoagulant
C. Massive hemolysis and cytokine release
D. Vitamin K deficiency
✅ Answer: C
31. Reticulocyte count is increased in:
A. Acute hemolysis only
B. Delayed hemolytic reaction
C. FNHTR
D. Allergic reaction
✅ Answer: B
32. Which is NOT an immune-mediated transfusion reaction?
A. AHTR
B. DHTR
C. TACO
D. FNHTR
✅ Answer: C
33. Most fatal transfusion reactions are due to:
A. Laboratory testing error
B. Clerical error
C. Storage lesion
D. Expired blood
✅ Answer: B
34. Which antibody activates complement most efficiently?
A. IgG
B. IgA
C. IgE
D. IgM
✅ Answer: D
35. Raised LDH in transfusion reaction indicates:
A. Liver failure
B. RBC destruction
C. Infection
D. Renal failure
✅ Answer: B
36. Hypocalcemia in massive transfusion is due to:
A. Potassium
B. Citrate
C. Heparin
D. EDTA
✅ Answer: B
37. Hyperkalemia in transfusion is seen due to:
A. RBC lysis during storage
B. Plasma proteins
C. Citrate metabolism
D. Leukocytes
✅ Answer: A
38. Which investigation differentiates TRALI from TACO?
A. DAT
B. Chest X-ray
C. Cardiac function assessment
D. Blood culture
✅ Answer: C
39. Which transfusion reaction presents with urticaria and itching only?
A. FNHTR
B. Allergic reaction
C. TRALI
D. Septic reaction
✅ Answer: B
40. In septic transfusion reaction, blood culture is taken from:
A. Patient only
B. Donor unit only
C. Both patient and donor unit
D. Environment only
✅ Answer: C
41. Which is a delayed complication of transfusion?
A. TRALI
B. FNHTR
C. Alloimmunization
D. Anaphylaxis
✅ Answer: C
42. The most reliable method to prevent ABO mismatch is:
A. Antibody screening
B. Leukoreduction
C. Proper patient identification
D. Washed RBCs
✅ Answer: C
43. TRALI pulmonary edema is due to:
A. Increased hydrostatic pressure
B. Left ventricular failure
C. Capillary leak syndrome
D. Fluid overload
✅ Answer: C
44. Which transfusion reaction has the highest mortality?
A. FNHTR
B. Allergic reaction
C. TRALI
D. Delayed hemolysis
✅ Answer: C
45. Hemovigilance refers to:
A. Blood donation
B. Monitoring transfusion reactions
C. Crossmatching
D. Blood storage
✅ Answer: B
46. The most common transfusion reaction overall is:
A. AHTR
B. FNHTR
C. TRALI
D. Septic reaction
✅ Answer: B
47. Which test helps detect DIC?
A. ESR
B. Bleeding time
C. D-dimer
D. Hemoglobin
✅ Answer: C
48. Mechanical hemolysis is caused by:
A. Antibodies
B. Cytokines
C. Faulty transfusion equipment
D. Plasma proteins
✅ Answer: C
49. The most effective preventive measure for FNHTR is:
A. Washed RBCs
B. Leukocyte-reduced blood
C. Male-only plasma
D. Irradiated blood
✅ Answer: B
50. The single most important step to reduce transfusion reaction-related mortality is:
A. Expensive testing
B. Early diagnosis and prompt action
C. Universal plasma transfusion
D. Massive transfusion protocols
✅ Answer: B