Introduction
- Intestinal protozoa infections caused by Entamoeba histolytica (responsible for amoebiasis) and Giardia lamblia (causing giardiasis) are significant public health concerns worldwide.
- These infections result from protozoan parasites that inhabit the gastrointestinal tract, leading to diarrhea, abdominal discomfort, malabsorption, and, in severe cases, life-threatening complications.
- Both organisms share similarities in transmission, primarily via the fecal-oral route, but differ in their life cycles, pathogenesis, and clinical manifestations.
- This article explains the introduction, geographical distribution, habitat, morphology, life cycle, transmission mode, incubation time, pathogenesis, laboratory diagnosis, and treatment of these two major intestinal protozoan infections.
Geographical Distribution
Amoeba (Entamoeba histolytica)
-
- Worldwide distribution, but most prevalent in tropical and subtropical regions with poor sanitation.
- The highest prevalence is in South Asia, Africa, and Central and South America.
- Common in travelers, refugees, and individuals in institutionalized settings.
Giardia (Giardia lamblia)
-
- Found globally, with higher prevalence in low-income regions where sanitation is inadequate.
- Endemic in parts of Africa, South Asia, and Latin America.
- Outbreaks often occur in developed countries due to exposure to contaminated water supplies or recreational water.
Habitat
Amoeba
-
- Trophozoite stage: Resides in the large intestine, feeding on bacteria and tissue.
- Cyst stage: Found in the colon and excreted in feces, surviving in the environment for extended periods.
Giardia
-
- Trophozoite stage: Attaches to the mucosa of the small intestine, primarily the duodenum and jejunum.
- Cyst stage: Forms in the colon and is shed in feces, surviving in external environments such as water and soil.
Morphology
Amoeba (Entamoeba histolytica)
-
- Trophozoite:
- Amoeboid shape, measuring 10–60 µm.
- Contains a single nucleus with a central karyosome.
- Engulfs red blood cells (erythrophagocytosis), a diagnostic feature.
- Cyst:
- Spherical, 10–20 µm in diameter.
- Contains 1–4 nuclei and chromatoid bodies.
- Trophozoite:
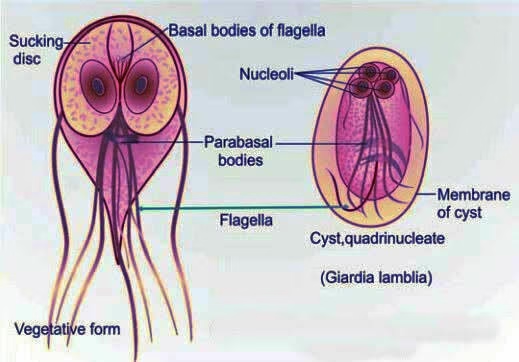
Giardia (Giardia lamblia)
-
- Trophozoite:
- Pear-shaped, 9–21 µm long and 5–15 µm wide.
- Binucleate with a ventral adhesive disc and four pairs of flagella.
- Cyst:
- Oval, 8–14 µm in length, with a thick wall.
- Contains four nuclei when mature.
- Trophozoite:
Life Cycle
Amoeba
-
- Ingestion: Cysts are ingested via contaminated water, food, or hands.
- Excystation: Cysts release trophozoites in the small intestine.
- Colonization: Trophozoites colonize the colon, feeding on host tissue.
- Encystation: Trophozoites form cysts in the large intestine.
- Excretion: Cysts are passed in feces and remain infectious in the environment.
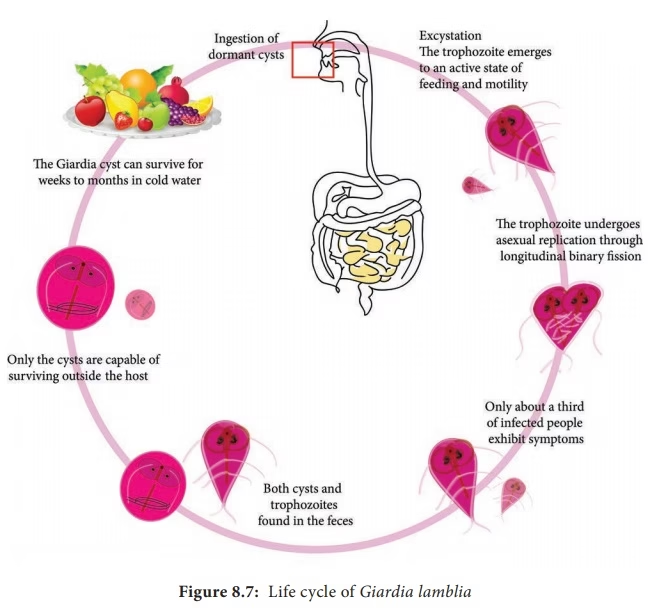
Giardia
-
- Ingestion: Cysts are ingested through contaminated water, food, or direct contact.
- Excystation: Gastric acid stimulates the release of trophozoites in the duodenum.
- Colonization: Trophozoites attach to the intestinal mucosa and multiply by binary fission.
- Encystation: Trophozoites form cysts in the colon.
- Excretion: Cysts are excreted in feces and survive in the environment.
Mode of Transmission
Both Entamoeba histolytica and Giardia lamblia share similar transmission routes:
-
- Fecal-oral route:
- Ingestion of contaminated food, water, or hands.
- Common in areas with poor sanitation and hygiene.
- Person-to-person contact:
- Transmission in daycare centers, households, and institutional settings.
- Sexual transmission via oral-anal contact.
- Zoonotic transmission (Giardia only):
- Contact with infected animals, such as beavers or dogs.
- Fecal-oral route:
Incubation Time
-
- Amoeba (Entamoeba histolytica): 1–4 weeks after ingestion of cysts.
- Giardia (Giardia lamblia): 1–2 weeks (commonly 7–10 days).
Pathogenesis
Amoeba
-
- Trophozoites invade the colonic mucosa, causing necrosis and ulceration.
- Severe cases lead to extraintestinal spread, especially to the liver (amoebic liver abscess).
- Clinical manifestations:
- Intestinal: Dysentery, abdominal pain, and bloody diarrhea.
- Extraintestinal: Liver abscess (fever, right upper quadrant pain), pleuropulmonary amoebiasis, and brain involvement (rare).
Giardia
-
- Trophozoites attach to the small intestinal mucosa, disrupting the epithelial barrier and causing malabsorption.
- Villous atrophy and enzyme deficiencies (e.g., lactase) exacerbate symptoms.
- Clinical manifestations:
- Acute: Watery diarrhea, bloating, flatulence, nausea, and abdominal cramps.
- Chronic: Malabsorption, weight loss, and fatigue.
- Asymptomatic carriers: Shed cysts without symptoms.
Laboratory Diagnosis
Amoeba
-
- Microscopy:
- Detection of trophozoites or cysts in stool samples.
- Trophozoites with ingested red blood cells confirm invasive infection.
- Antigen detection:
- ELISA or immunochromatographic tests for E. histolytica-specific antigens.
- Molecular methods:
- PCR to differentiate E. histolytica from nonpathogenic species like E. dispar.
- Serology:
- Useful for extraintestinal amoebiasis (e.g., liver abscess).
- Imaging:
- Ultrasound or CT for liver abscess diagnosis.
- Microscopy:
Giardia
-
- Microscopy:
- Direct stool examination for cysts or trophozoites.
- Concentration techniques enhance sensitivity.
- Antigen detection:
- ELISA or rapid immunoassays for Giardia-specific antigens in stool.
- Molecular methods:
- PCR for detecting Giardia DNA in stool.
- String test (Enterotest):
- Collection of duodenal contents for analysis.
- Microscopy:
Treatment
Amoeba
-
- Amoebic colitis or dysentery:
- Metronidazole (750 mg three times daily for 7–10 days) or Tinidazole (2 g daily for 3 days).
- Asymptomatic cyst carriers:
- Paromomycin or iodoquinol to eliminate cysts.
- Amoebic liver abscess:
- Drainage in severe cases, combined with metronidazole or tinidazole.
- Amoebic colitis or dysentery:
Giardia
-
- First-line treatment:
- Metronidazole (250 mg three times daily for 5–7 days) or Tinidazole (single 2 g dose).
- Alternative drugs:
- Nitazoxanide, Albendazole, or Furazolidone for resistant cases or intolerance to metronidazole.
- Supportive care:
- Rehydration therapy and dietary modifications (e.g., avoiding lactose).
- First-line treatment:
Prevention and Control
-
- Improve sanitation:
- Access to clean water and proper sewage disposal.
- Promote hygiene:
- Regular handwashing and proper food handling.
- Water treatment:
- Boiling, filtration, or chemical disinfection of drinking water.
- Public health measures:
- Education campaigns and screening in high-risk populations.
- Improve sanitation: