- Cytochemical staining procedures are essential laboratory techniques for diagnosing and classifying hematopoietic disorders, including leukemias and other blood-related diseases.
- These stains help differentiate cell types based on their biochemical properties, identifying specific cell lineages, maturation stages, and pathologies.
- Below, we’ll discuss various cytochemical staining procedures and their applications in hematopoietic disorders.
Cytochemical Staining Procedures
- Cytochemical staining is a cornerstone of hematopathology, particularly for classifying and diagnosing various hematological disorders, including leukemias, lymphomas, and anemias.
- Each staining technique targets specific cellular components, enhancing the identification of distinct cell types and their pathologies.
Myeloperoxidase (MPO) Staining
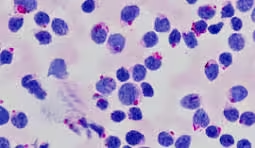
- Purpose: Differentiates myeloid cells from lymphoid cells and identifies acute myeloid leukemia (AML).
- Mechanism: Myeloperoxidase is an enzyme found in azurophilic granules of myeloid cells (granulocytes). In this staining procedure, a substrate is introduced that catalyzes a reaction in the presence of MPO, producing a colored end product (often brown).
- Procedure:
- Prepare a smear from the bone marrow or peripheral blood.
- Fix the smear and incubate it in a solution containing the substrate for MPO (typically a combination of hydrogen peroxide and a dye).
- Rinse and visualize under a microscope.
- Interpretation:
- Positive Result: Granulocytes and myeloblasts stain brown, indicating the presence of myeloid lineage.
- Negative Result: Lymphocytes and some other cells do not stain, which helps in differentiating AML from ALL.
- Clinical Relevance: MPO positivity in greater than 20% of blasts indicates AML, while a negative result suggests ALL.
Sudan Black B (SBB) Staining
- Purpose: Identifies cell lipid content, primarily to confirm myeloid lineage.
- Mechanism: Sudan Black B stains neutral lipids and phospholipids within the cytoplasm. The dye is lipophilic and selectively binds to lipid components.
- Procedure:
- Prepare a smear from bone marrow or blood and air dry.
- Fix in a fixative, followed by incubation in a solution containing Sudan Black B.
- Rinse and observe under a microscope.
- Interpretation:
- Positive Result: Granulocytes and monocytes stain dark blue or black, while lymphocytes remain unstained.
- Negative Result: Indicates non-myeloid lineage.
- Clinical Relevance: SBB is often used alongside MPO staining to confirm AML, particularly in distinguishing myeloid leukemias from lymphoid leukemias.
Esterase Staining
- Purpose: Differentiates myeloid from monocytic lineages and helps classify acute leukemias.
- Types of Esterase Staining:
- Naphthol AS-D Chloroacetate Esterase (CAE): This stain is specific for myeloid cells.
- Alpha-Naphthyl Butyrate Esterase (NBE): This stain is used to identify monocytic cells.
- Mechanism: Each type of esterase acts on a specific substrate, producing a colored product.
- Procedure:
- Prepare a smear and fix it.
- Incubate the smear in a solution containing the respective substrate for the esterase.
- Rinse and visualize under a microscope.
- Interpretation:
- CAE Positive: Indicates myeloid lineage (e.g., myeloblasts).
- NBE Positive: Indicates monocytic lineage (e.g., monoblasts).
- Clinical Relevance: This staining helps accurately classify acute leukemias, particularly differentiating AML from acute monoblastic leukemia (AMoL).
Periodic Acid-Schiff (PAS) Staining
- Purpose: Identifies glycogen and polysaccharides, which are useful in diagnosing certain types of leukemias and assessing the maturation of cells.
- Mechanism: Periodic acid oxidizes vicinal diols in carbohydrates to aldehydes, reacting with Schiff reagent to produce a pink or magenta color.
- Procedure:
- Prepare a smear and fix it.
- Treat the smear with periodic acid followed by Schiff reagent.
- Rinse and examine under a microscope.
- Interpretation:
- Positive Result: Cells rich in glycogen, such as myeloblasts in acute myeloblastic leukemia, will appear magenta.
- Negative Result: Indicates a lack of glycogen, aiding in further classification.
- Clinical Relevance: PAS positivity is particularly helpful in diagnosing acute lymphoblastic leukemia (ALL) and distinguishing between myeloid and lymphoid leukemias.
Toluidine Blue O Staining
- Purpose: Identifies mast cells and aids in diagnosing mast cell disorders.
- Mechanism: Toluidine Blue O is a metachromatic stain that binds to mast cells’ heparin and other granule contents, resulting in a distinct color change.
- Procedure:
- Prepare the smear and fix it.
- Stain with Toluidine Blue O for a specified time.
- Rinse and visualize under a microscope.
- Interpretation:
- Positive Result: Mast cells stain blue, while other cell types will not exhibit the same color intensity.
- Clinical Relevance: Used to confirm mastocytosis and assess the number of mast cells in various hematological disorders.
Reticulocyte Staining
- Purpose: Evaluate the production of reticulocytes, providing insights into bone marrow activity and erythropoiesis.
- Mechanism: Supravital stains (e.g., New Methylene Blue or Brilliant Cresyl Blue) stain RNA within reticulocytes, allowing them to be distinguished from mature red blood cells.
- Procedure:
- A blood smear is prepared and air-dried.
- The smear is stained with New Methylene Blue for a specified time.
- Rinse and observe under a microscope.
- Interpretation:
- Positive Result: Reticulocytes appear blue or greenish due to the residual RNA, indicating active erythropoiesis.
- Clinical Relevance: Reticulocyte counts are crucial in evaluating responses to anemia and the effectiveness of treatment.
Iron Staining (Prussian Blue Staining)
- Purpose: Identifying iron deposits in cells is crucial for diagnosing iron deficiency anemia and iron overload disorders.
- Mechanism: Ferric iron reacts with potassium ferricyanide to produce a blue-colored complex.
- Procedure:
- Prepare a smear and fix it.
- Stain with Prussian Blue solution, then rinse and observe.
- Interpretation:
- Positive Result: Iron deposits are visualized as blue granules within cells, indicating iron overload or sideroblastic anemia.
- Clinical Relevance: Essential for evaluating iron metabolism disorders, including hereditary hemochromatosis and sideroblastic anemia.
Cytochemical Markers in Acute and Chronic Leukemias
Different cytochemical stains are routinely used to characterize various types of leukemia based on specific cytological features:
- Acute Myeloid Leukemia (AML): Typically shows positivity for MPO, SBB, and CAE. PAS may show mixed results depending on the subtype.
- Acute Lymphoblastic Leukemia (ALL): Generally negative for MPO and SBB, with possible PAS positivity depending on the subtype.
- Chronic Myeloid Leukemia (CML): Characterized by the presence of myeloid cells; cytogenetic studies confirm the Philadelphia chromosome.
- Chronic Lymphocytic Leukemia (CLL): Flow cytometry is often used alongside cytochemical staining to confirm the diagnosis based on specific surface markers.
Summary of Cytochemical Staining Techniques
| Staining Technique | Purpose | Key Features |
| Myeloperoxidase (MPO) | Differentiate myeloid vs. lymphoid lineage | Positive in myeloid cells (AML) |
| Sudan Black B (SBB) | Identify lipid content | Positive in myeloid cells (granulocytes) |
| Esterase Staining | Differentiate myeloid and monocytic lineage | CAE positive for myeloid; NBE positive for mono |
| Periodic Acid-Schiff (PAS) | Identify glycogen and polysaccharides | Positive in certain myeloblasts and lymphoblasts |
| Toluidine Blue O | Identify mast cells | Stains mast cells blue |
| Reticulocyte Staining | Assess erythropoiesis | Reticulocytes stain blue due to RNA |
| Iron Staining (Prussian Blue) | Identify iron deposits | Positive indicates iron overload |
Clinical Implications of Cytochemical Staining
Cytochemical staining procedures are vital for accurately diagnosing and classifying hematological malignancies, influencing treatment strategies and patient outcomes.
The specificity of these stains allows clinicians to determine the lineage and maturation stage of cells, leading to more tailored and effective treatment options. For example:
- Targeted Therapies: Knowledge of specific genetic mutations and cellular characteristics can guide targeted therapies such as tyrosine kinase inhibitors in CML or monoclonal antibodies in CLL.
- Monitoring Disease Progression: Staining procedures can help monitor response to treatment, detect minimal residual disease, and inform prognosis based on cytological features.