Introduction
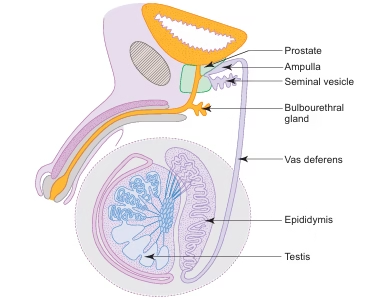
The male reproductive system consists of specialized organs that are responsible for the production, maturation, and transport of male gametes and hormones.
It includes the following structures:
-
Testes
-
A pair of testes act as the primary male sex glands and are located in the scrotum.
-
They produce male gametes called spermatozoa.
-
They also secrete the male sex hormone testosterone.
-
-
Genital ducts
-
These include the epididymis, vas deferens, and ejaculatory duct.
-
Their function is to conduct sperms to the urethra.
-
During passage through the duct system, especially the epididymis, sperms mature and become motile.
-
Smooth muscle in the duct walls contracts during ejaculation to expel sperms.
-
-
Accessory sex glands
-
These include a pair of seminal vesicles, a single prostate gland, and a pair of bulbourethral glands.
-
They secrete seminal fluid, which acts as a transport medium and provides nourishment to sperms.
-
The structure and function of these glands depend on testosterone.
-
-
Penis
-
The penis functions as the organ of copulation.
-
Testis
General architecture of the testis
-
Unlike the ovary, the testes are located outside the body in the scrotum.
-
The scrotal temperature is about 2–3°C lower than body temperature, which is essential for normal spermatogenesis.
-
Each testis is oval in shape and measures approximately 5 cm in length and 2.5 cm in width.
-
The weight of each testis ranges from 10 to 15 g.
-
Tunica vaginalis
-
Each testis is surrounded, except at the posterior border, by a serous sac called the tunica vaginalis.
-
It is derived from the peritoneum during the descent of the testis.
-
-
Tunica albuginea
-
Deep to the tunica vaginalis is a thick white fibrous connective tissue capsule called the tunica albuginea.
-
It completely encloses the testis.
-
Along the posterior border, it thickens and projects inward to form the mediastinum testis.
-
-
Lobules of testis
-
Thin fibrous septa extend from the mediastinum testis to the tunica albuginea.
-
These septa divide the testis into several compartments called lobules.
-
Each lobule contains one to four highly coiled seminiferous tubules.
-
-
Tunica vasculosa
-
Internal to the tunica albuginea lies a layer of vascular loose connective tissue known as the tunica vasculosa.
-
It extends into the interior as interstitial connective tissue surrounding the seminiferous tubules.
-
This connective tissue contains clusters of interstitial cells of leydig, which secrete testosterone.
-
-
Rete testis and straight tubules
-
The mediastinum testis contains a network of irregular channels called the rete testis.
-
Seminiferous tubules connect to the rete testis through short straight tubules.
-
Straight tubules are lined by cuboidal or low columnar epithelium.
-
Rete testis is lined by simple squamous or cuboidal epithelium.
-
-
Efferent ductules
-
The rete testis connects to the epididymis through 10–15 efferent ductules.
-
These ductules emerge from the upper part of the testis.
-
They are lined by epithelium composed of cells of different heights, giving the lumen an uneven contour.
-
Tall columnar cells possess cilia, while short cuboidal cells contain microvilli.
-
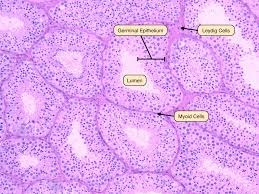
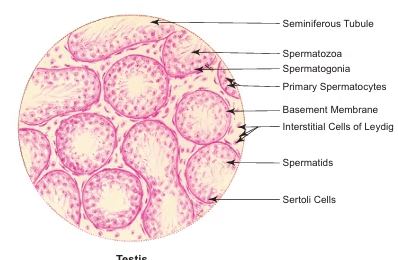
Seminiferous tubules
-
Seminiferous tubules are highly coiled and tightly packed tubules present within the testis.
-
Each seminiferous tubule measures approximately 50–80 cm in length and 150–250 μm in diameter.
-
These tubules are the sites of spermatozoa production through the process known as spermatogenesis.
-
Seminiferous tubules are lined by a specialized stratified germinal epithelium, also called the seminiferous epithelium.
-
Seminiferous epithelium
-
The epithelium consists of two distinct populations of cells.
-
Spermatogenic cells, which are directly involved in spermatogenesis.
-
Sertoli cells, which provide structural support and nourishment to developing spermatozoa.
-
This specialized epithelium rests on a basement membrane.
-
Beneath the basement membrane are slender contractile smooth muscle–like cells called myoid cells.
-
Spermatogenic cells
-
Spermatogenic cells are arranged in an orderly developmental sequence from the basement membrane toward the lumen.
-
The stages include spermatogonia, spermatocytes, spermatids, and finally spermatozoa.
-
The process by which spermatogonia divide, differentiate, and mature into spermatozoa is termed spermatogenesis.
-
Spermatogenesis occurs in waves along the length of the seminiferous tubules.
-
In humans, the complete process takes approximately 64 ± 4 days.
-
Spermatogonia
-
Spermatogonia are immature spermatogenic cells located on the basement membrane of the seminiferous tubules.
-
They undergo mitotic division to form two types of cells.
-
Type A sper spermatogonia have darkly stained nuclei and function as stem cells of the germinal epithelium.
-
Type B spermatogonia have lightly stained nuclei and undergo further maturation.
-
Type B spermatogonia differentiate to form primary spermatocytes.
-
Genital ducts
-
Genital ducts are responsible for conducting sperms to the urethra.
-
The genital duct system includes the epididymis, ductus deferens, and ejaculatory duct.
Epididymis
-
The epididymis is a comma-shaped structure located on the posterolateral aspect of the testis.
-
It is composed of a highly coiled tube called the ductus epididymis.
-
The ductus epididymis measures approximately 6 m in length.
-
It is supported by vascular connective tissue.
-
The epididymis is divided into three parts: head, body, and tail.
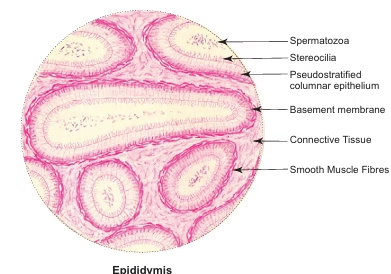
-
Histological features
-
The ductus epididymis is lined by pseudostratified columnar epithelium.
-
This epithelium consists of two types of cells.
-
Tall columnar principal cells.
-
Small basal cells.
-
The tall columnar principal cells bear long microvilli known as stereocilia.
-
These cells are involved in both secretion and absorption.
-
-
Muscle layer
-
Beneath the epithelium lies a layer of circularly arranged smooth muscle fibers.
-
The thickness of this muscle layer gradually increases from the head to the tail.
-
In the tail region, the muscle may be organized into inner circular and outer longitudinal layers.
-
The smooth muscle is richly innervated by sympathetic fibers.
-
Intense rhythmic contractions of this muscle help in the expulsion of sperms during ejaculation.
-
-
Functions of epididymis
-
Storage of spermatozoa, mainly in the tail of the epididymis.
-
Maturation of spermatozoa, during which they acquire motility.
-
Absorption of testicular fluid, with approximately 90% of the fluid being absorbed.
-
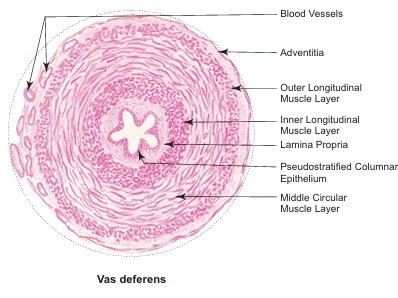
Vas deferens (ductus deferens)
-
The ductus deferens is a thick, muscular tube extending from the tail of the epididymis to the prostatic urethra.
-
The distal end of the ductus deferens is dilated to form the ampulla.
-
The ampulla joins with the duct of the seminal vesicle to form the ejaculatory duct.
-
The ejaculatory duct from each side passes through the prostate gland.
-
It opens into the prostatic urethra.
-
Structure of the wall
-
The wall of the ductus deferens is composed of three distinct coats.
-
-
Mucosa
-
The mucosa consists of a pseudostratified columnar epithelial lining.
-
It is supported by an underlying lamina propria.
-
The epithelial cells possess stereocilia.
-
The mucosa is thrown into longitudinal folds.
-
These folds allow expansion of the duct during ejaculation.
-
-
Muscle layer
-
The muscle layer is composed of smooth muscle fibers.
-
The fibers are arranged into three layers.
-
Inner longitudinal layer.
-
Middle circular layer, which is the thickest.
-
Outer longitudinal layer.
-
-
-
Adventitia
-
The outermost layer is the adventitia.
-
It is composed of fibroelastic connective tissue.
-
It contains blood vessels and nerves.
-
Ejaculatory duct
-
Ejaculatory ducts are two in number.
-
Each ejaculatory duct measures approximately 2 cm in length.
-
Each duct is formed by the union of the duct of the seminal vesicle and the ampulla of the vas deferens.
-
After formation, the ejaculatory duct passes through the substance of the prostate gland.
-
It runs lateral to the prostatic utricle.
-
The ejaculatory duct opens into the prostatic urethra.
-
It is lined by simple columnar epithelium.
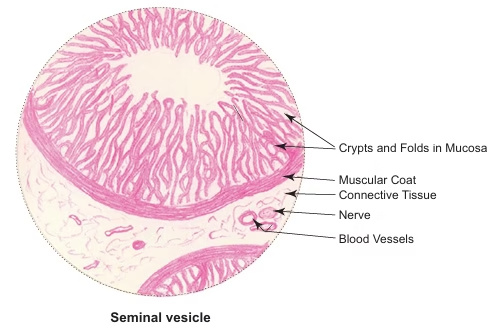
Seminal vesicle
-
Seminal vesicles are paired accessory sex glands located at the base of the urinary bladder.
-
Each seminal vesicle is an elongated blind tube measuring about 12–15 cm in length.
-
The tube is highly coiled upon itself, reducing its overall size to approximately 5 cm.
-
In histological sections, the same tube is seen cut at different orientations due to its coiled nature.
-
Secretions
-
Seminal vesicles secrete a thick, yellow, viscous, alkaline fluid.
-
The secretion is rich in fructose, which serves as a major energy source for sperms.
-
It also contains ascorbic acid and prostaglandins.
-
-
Structure of the wall
-
The wall of the seminal vesicle is composed of three coats.
-
-
Mucosa
-
The mucosa is thrown into complex folds.
-
These folds branch and anastomose to form crypts and cavities.
-
This arrangement gives a characteristic honeycomb appearance to the lumen.
-
The mucosal epithelium is secretory in nature.
-
It is predominantly pseudostratified low columnar epithelium.
-
In some regions, the epithelium may appear simple columnar or cuboidal, depending on the level of secretory activity.
-
The lamina propria is rich in elastic fibers.
-
It extends into and supports the mucosal folds.
-
-
Muscle layer
-
The muscle layer is composed of smooth muscle fibers.
-
These fibers are arranged into two layers.
-
Inner circular layer.
-
Outer longitudinal layer.
-
-
Contraction of the muscle layer helps in expressing the glandular secretion into the urethra through the ejaculatory duct.
-
-
Adventitia
-
The outermost layer is the adventitia.
-
It is made of loose connective tissue.
-
It contains blood vessels and nerves.
-
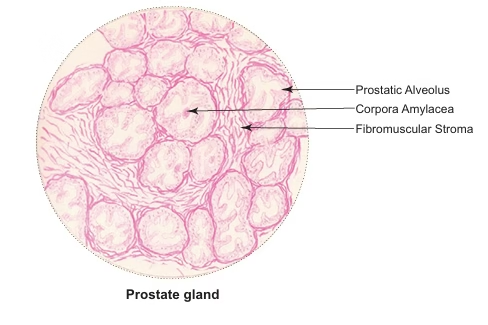
Prostate
-
The prostate is the largest accessory sex gland in males.
-
It surrounds the beginning of the male urethra.
-
In an adult male, it is approximately the size of a chestnut.
-
It weighs about 20 g.
-
General structure
-
The prostate is composed of 30–50 branched tubuloalveolar glands.
-
These glands are embedded in a fibromuscular stroma.
-
The ducts of the glands open into the prostatic urethra.
-
-
Capsules of prostate
-
The prostate is enclosed by two capsules.
-
The true capsule is formed by condensation of the fibromuscular stroma at the periphery.
-
The false capsule is formed by the pelvic fascia.
-
A rich venous plexus is present between the true and false capsules.
-
-
Secretions
-
The prostate secretes a thin, milky fluid.
-
The secretion is rich in citric acid, acid phosphatase, amylase, and fibrinolysin.
-
Fibrinolysin helps in liquefaction of coagulated semen after ejaculation.
-
Prostatic secretion forms approximately 75% of the seminal fluid.
-
Serum prostate specific antigen (psa) levels are increased in patients with prostatic tumors.
-
-
Arrangement of prostatic glands
-
Prostatic glands are arranged concentrically around the urethra.
-
They are divided into three groups.
-
Mucosal glands.
-
Submucosal glands.
-
Main glands.
-
-
Mucosal glands are small tubular glands located in the inner zone.
-
They open directly into the urethra.
-
Submucosal glands are tubuloalveolar glands located in the intermediate zone.
-
Main glands are tubuloalveolar glands present in the outer zone.
-
Submucosal and main glands open into the prostatic sinus of the urethra through long ducts.
-
-
Histological features
-
Histologically, the prostate consists of parenchyma and fibromuscular stroma.
-
The parenchyma is formed by large irregular prostatic alveoli with wide lumina.
-
The secretory epithelium lining the alveoli varies from cuboidal to columnar depending on secretory activity.
-
The lumen may contain spherical prostatic concretions known as corpora amylacea.
-
These concretions are formed by condensation of prostatic secretions.
-
The number of prostatic concretions increases with age and may undergo calcification.
-
-
Fibromuscular stroma
-
The fibromuscular stroma provides support to the parenchyma.
-
It is composed of smooth muscle fibers mixed with connective tissue fibers.
-
The fibers run in different directions.
-
The stroma also contains blood vessels, lymphatics, and nerves.
-
-
Prostatic urethra
-
The prostatic urethra within the prostate is crescent-shaped.
-
It shows multiple diverticula or outpocketings.
-
The upper part is lined by transitional epithelium.
-
The lower part is lined by stratified columnar epithelium.
-
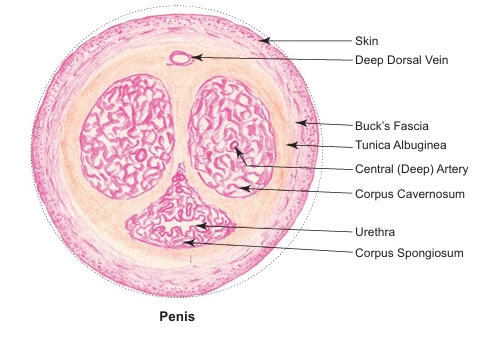
Penis
Gross features
-
The penis is an erectile male organ of copulation.
-
It is cylindrical in shape.
-
During erection, it becomes enlarged, elongated, and turgid.
-
Erectile bodies
-
The penis is composed of three cylindrical masses of spongy cavernous tissue.
-
A pair of corpora cavernosa.
-
A single corpus spongiosum.
-
The corpora cavernosa are positioned side by side on the dorsal aspect of the penis.
-
Each corpus cavernosum is traversed by the deep artery of the penis.
-
-
Corpus spongiosum and glans
-
The corpus spongiosum is located ventrally.
-
It is traversed by the penile urethra.
-
Distally, the corpora cavernosa end blindly beneath the glans penis.
-
The glans penis is the enlarged cap-like terminal part of the corpus spongiosum.
-
The glans penis forms the tip of the penis.
-
It is covered by a retractable fold of skin called the prepuce.
-
The fossa navicularis of the urethra passes through the glans penis and opens at the external urethral meatus.
-
Microscopic structure
-
The erectile cavernous tissue of the corpora cavernosa and corpus spongiosum consists of endothelium-lined cavernous spaces.
-
These spaces are separated by trabeculae.
-
The trabeculae contain collagen fibers, elastic fibers, and smooth muscle fibers.
-
Blood supply and erection
-
The cavernous spaces receive blood from the dorsal and deep arteries of the penis.
-
Additional blood supply comes from the bulbourethral artery.
-
Blood drains from the cavernous spaces through the dorsal veins.
-
During erection, parasympathetic stimulation causes vasodilatation of arteries.
-
This results in filling and engorgement of cavernous spaces.
-
Engorgement compresses peripheral veins, reducing venous outflow and maintaining erection.
-
-
Penile urethra
-
The penile urethra has an irregular outline.
-
This is due to deep outpocketings known as sinuses of morgagni.
-
It is lined by stratified columnar epithelium.
-
The urethra is lubricated by mucous secretion from the paraurethral glands of littre.
-
These glands open into the outpocketings of the penile urethra.
-
-
Epithelial lining
-
The glans penis, external urethral meatus, and navicular fossa are lined by stratified squamous epithelium.
-
-
Tunica albuginea
-
The erectile bodies are enclosed by a fibrous sheath called the tunica albuginea.
-
The tunica albuginea consists of two layers.
-
An outer layer.
-
An inner layer.
-
The outer layer is composed of longitudinal collagen fibers.
-
It forms a common covering for all three erectile bodies.
-
MCQs
1. Seminiferous tubules are lined by:
A. Simple squamous epithelium
B. Simple columnar epithelium
C. Stratified germinal epithelium
D. Pseudostratified epithelium
Answer: C
2. Which cell forms the blood–testis barrier?
A. Spermatogonia
B. Myoid cells
C. Leydig cells
D. Sertoli cells
Answer: D
3. Interstitial cells of leydig are located in:
A. Lumen of seminiferous tubules
B. Tunica albuginea
C. Interstitial tissue between tubules
D. Rete testis
Answer: C
4. Hormone secreted by leydig cells is:
A. Estrogen
B. Progesterone
C. Testosterone
D. Inhibin
Answer: C
5. Myoid cells are present:
A. Inside seminiferous tubules
B. Beneath basement membrane
C. Inside rete testis
D. In epididymal lumen
Answer: B
6. Stereocilia are characteristically seen in:
A. Vas deferens
B. Seminiferous tubules
C. Epididymis
D. Ejaculatory duct
Answer: C
7. Epithelium of epididymis is:
A. Simple columnar
B. Stratified squamous
C. Pseudostratified columnar
D. Transitional
Answer: C
8. Principal cells of epididymis are involved in:
A. Phagocytosis
B. Spermatogenesis
C. Secretion and absorption
D. Hormone synthesis
Answer: C
9. Irregular lumen of epididymis is due to:
A. Mucosal folds
B. Stereocilia
C. Variable cell height
D. Muscular contraction
Answer: C
10. Which duct shows the thickest smooth muscle coat?
A. Epididymis
B. Vas deferens
C. Ejaculatory duct
D. Urethra
Answer: B
11. Muscle layers of vas deferens are:
A. One
B. Two
C. Three
D. Four
Answer: C
12. Thickest muscle layer of vas deferens is:
A. Inner longitudinal
B. Middle circular
C. Outer longitudinal
D. Adventitia
Answer: B
13. Epithelium of vas deferens is:
A. Simple columnar
B. Pseudostratified columnar with stereocilia
C. Stratified squamous
D. Transitional
Answer: B
14. Ejaculatory duct is formed by:
A. Epididymis and urethra
B. Vas deferens and prostate
C. Ampulla of vas deferens and seminal vesicle duct
D. Seminal vesicle and urethra
Answer: C
15. Epithelium of ejaculatory duct is:
A. Pseudostratified columnar
B. Stratified squamous
C. Simple columnar
D. Transitional
Answer: C
16. Seminal vesicle secretion is rich in:
A. Citric acid
B. Fructose
C. Testosterone
D. Urea
Answer: B
17. Lumen of seminal vesicle shows:
A. Smooth outline
B. Honeycomb appearance
C. Narrow lumen
D. Villi
Answer: B
18. Epithelium of seminal vesicle is:
A. Stratified squamous
B. Pseudostratified low columnar
C. Transitional
D. Simple squamous
Answer: B
19. Muscle layer of seminal vesicle consists of:
A. Only circular layer
B. Only longitudinal layer
C. Inner circular and outer longitudinal
D. Skeletal muscle
Answer: C
20. Largest accessory sex gland is:
A. Seminal vesicle
B. Bulbourethral gland
C. Prostate
D. Epididymis
Answer: C
21. Prostatic glands are:
A. Simple tubular
B. Alveolar
C. Tubuloalveolar
D. Compound tubular
Answer: C
22. Which substance liquefies coagulated semen?
A. Fructose
B. Citric acid
C. Fibrinolysin
D. Amylase
Answer: C
23. Corpora amylacea are seen in:
A. Seminal vesicle
B. Epididymis
C. Prostate
D. Testis
Answer: C
24. Corpora amylacea increase with:
A. Puberty
B. Infection
C. Age
D. Ejaculation
Answer: C
25. Fibromuscular stroma of prostate contains:
A. Skeletal muscle
B. Smooth muscle and connective tissue
C. Elastic cartilage
D. Adipose tissue
Answer: B
26. Upper part of prostatic urethra is lined by:
A. Stratified squamous epithelium
B. Transitional epithelium
C. Simple columnar epithelium
D. Pseudostratified epithelium
Answer: B
27. Penis contains how many erectile bodies?
A. One
B. Two
C. Three
D. Four
Answer: C
28. Corpora cavernosa are located on:
A. Ventral aspect
B. Dorsal aspect
C. Lateral aspect
D. Central region
Answer: B
29. Penile urethra passes through:
A. Corpora cavernosa
B. Corpus spongiosum
C. Tunica albuginea
D. Glans only
Answer: B
30. Erectile tissue is composed of:
A. Solid muscle mass
B. Cavernous spaces
C. Glandular tissue
D. Fat cells
Answer: B
31. Cavernous spaces are lined by:
A. Cuboidal epithelium
B. Columnar epithelium
C. Endothelium
D. Stratified epithelium
Answer: C
32. Erection of penis is mediated mainly by:
A. Sympathetic nerves
B. Parasympathetic nerves
C. Somatic nerves
D. Endocrine reflex
Answer: B
33. Tunica albuginea of penis is:
A. Muscular layer
B. Epithelial covering
C. Fibrous sheath
D. Serous membrane
Answer: C
34. Sinuses of morgagni are present in:
A. Prostatic urethra
B. Penile urethra
C. Membranous urethra
D. Bladder
Answer: B
35. Glands of littre secrete:
A. Enzymes
B. Testosterone
C. Mucus
D. Fructose
Answer: C
36. Glans penis is lined by:
A. Simple columnar epithelium
B. Pseudostratified epithelium
C. Stratified squamous epithelium
D. Transitional epithelium
Answer: C
37. Seminiferous tubules open into:
A. Epididymis directly
B. Efferent ductules
C. Rete testis via straight tubules
D. Vas deferens
Answer: C
38. Rete testis is lined by:
A. Stratified epithelium
B. Simple squamous or cuboidal epithelium
C. Pseudostratified epithelium
D. Transitional epithelium
Answer: B
39. Efferent ductules show:
A. Smooth lumen
B. Scalloped lumen
C. Collapsed lumen
D. Narrow lumen
Answer: B
40. Cilia in efferent ductules are present on:
A. Cuboidal cells
B. Basal cells
C. Columnar cells
D. Myoid cells
Answer: C
41. Primary function of epididymis is:
A. Hormone secretion
B. Spermatogenesis
C. Sperm maturation and storage
D. Ejaculation
Answer: C
42. Basement membrane of seminiferous tubules supports:
A. Leydig cells
B. Sertoli cells and spermatogonia
C. Spermatozoa
D. Rete testis
Answer: B
43. Spermatogenesis occurs in:
A. Epididymis
B. Seminiferous tubules
C. Rete testis
D. Vas deferens
Answer: B
44. Duration of spermatogenesis in humans is:
A. 30 days
B. 45 days
C. 64 days
D. 90 days
Answer: C
45. Tunica vaginalis is derived from:
A. Mesentery
B. Pelvic fascia
C. Peritoneum
D. Endoderm
Answer: C
46. Mediastinum testis contains:
A. Seminiferous tubules
B. Rete testis
C. Leydig cells
D. Vas deferens
Answer: B
47. Efferent ductules connect:
A. Seminiferous tubules to vas deferens
B. Rete testis to epididymis
C. Epididymis to vas deferens
D. Prostate to urethra
Answer: B
48. Predominant muscle type in male reproductive ducts is:
A. Skeletal muscle
B. Cardiac muscle
C. Smooth muscle
D. Elastic tissue
Answer: C
49. Sympathetic stimulation is important for:
A. Erection
B. Ejaculation
C. Spermatogenesis
D. Hormone secretion
Answer: B
50. Prostate specific antigen is produced by:
A. Seminal vesicle
B. Sertoli cells
C. Prostate
D. Leydig cells
Answer: C