- Identifying microorganisms within tissue samples is crucial in diagnosing infectious diseases and determining their causative agents.
- Microorganisms, such as bacteria, fungi, viruses, and parasites, are often visualized in tissue histological sections through various staining techniques.
- Each staining method is tailored to highlight specific microbial characteristics, such as cell wall composition, morphology, or presence of certain proteins, to differentiate between microbial types and aid in diagnosis.
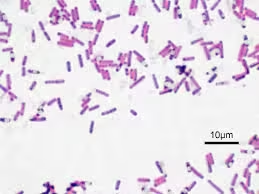
Gram Stain
The Gram stain is one of the most widely used techniques in microbiology for distinguishing between Gram-positive and Gram-negative bacteria based on their cell wall structure.
Principle:
Gram-positive bacteria retain the crystal violet stain due to their thick peptidoglycan layer. In contrast, Gram-negative bacteria, with a thinner peptidoglycan layer and an outer lipid membrane, do not retain the crystal violet stain and instead take up the counterstain.
Materials:
- Crystal violet stain
- Gram’s iodine (mordant)
- Decolorizer (ethanol or acetone)
- Safranin or fuchsin (counterstain)
- Microscope slides
Procedure:
- Fix the tissue section on a slide by heating gently or using formalin fixation.
- Flood the slide with crystal violet and let sit for 1 minute.
- Rinse with distilled water.
- Apply Gram’s iodine for 1 minute to form the crystal violet-iodine complex.
- Rinse with water.
- Decolorize with ethanol or acetone for 10-30 seconds (or until color stops running).
- Rinse immediately with water to stop the decolorization process.
- Counterstain with safranin or fuchsin for 1 minute.
- Rinse with water and blot dry.
- Examine under a microscope. Gram-positive bacteria will appear purple, and Gram-negative bacteria will appear pink or red.
Interpretation: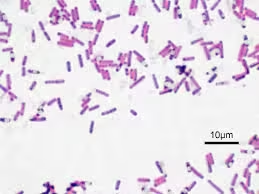
Gram-positive bacteria appear purple, while Gram-negative bacteria appear red or pink.
Applications:
Useful in distinguishing bacterial types in tissue sections, aiding in diagnosing bacterial infections.
Acid-Fast Stain (Ziehl-Neelsen and Kinyoun Stains)
Acid-fast staining is specifically designed to detect Mycobacterium species, such as Mycobacterium tuberculosis, due to their waxy, lipid-rich cell walls that resist conventional staining.
Principle:
Acid-fast bacteria retain the primary stain despite being treated with acid-alcohol, which would typically decolorize non-acid-fast cells.
Materials:
- Carbol fuchsin stain
- Acid-alcohol (decolorizer)
- Methylene blue or malachite green (counterstain)
- Heat source
Procedure:
- Fix the tissue section on a slide.
- Cover the slide with carbol fuchsin stain.
- Heat gently (do not boil) for 3-5 minutes to allow the stain to penetrate.
- Rinse with water.
- Decolorize with acid-alcohol until no color runs off (about 30 seconds).
- Rinse with water.
- Counterstain with methylene blue or malachite green for 1-2 minutes.
- Rinse with water, blot dry, and examine under a microscope. Acid-fast bacteria will appear bright pink, while other cells will appear blue or green.
Interpretation:
Acid-fast bacteria appear bright red or pink against a blue or green background.
Applications:
Primarily used to detect Mycobacterium species in tissue sections, but also effective for other acid-fast organisms like Nocardia and some parasites.
Silver Stains (Gomori Methenamine Silver – GMS)
Silver staining methods, including the Gomori Methenamine Silver (GMS) stain, are effective for highlighting fungi and certain bacteria due to their affinity for silver ions.
Principle:
Fungal cell walls and certain bacterial organisms reduce silver ions to metallic silver, resulting in dark or black-stained microorganisms against a lighter background.
Materials:
- Chromic acid (oxidizer)
- Methenamine silver solution
- Sodium borate solution
- Gold chloride (toner)
- Light green counterstain (optional)
Procedure:
- Deparaffinize and hydrate tissue sections.
- Oxidize with chromic acid for 10 minutes, then rinse with water.
- Rinse in sodium bisulfite solution for 1 minute to remove excess chromic acid, then rinse with water.
- Immerse in methenamine silver solution at 60°C for 10-15 minutes.
- Rinse in distilled water.
- Tone with gold chloride solution for a few seconds.
- Rinse with water, then place in sodium thiosulfate for 1 minute to remove unreacted silver.
- Rinse and counterstain with light green if desired.
- Rinse, dehydrate, and mount for microscopic examination. Fungi will appear black, while tissue will be light green or yellowish.
Interpretation:
Fungal hyphae, yeast forms, and certain bacteria (e.g., Legionella, H. pylori) appear black against a light green or yellow background.
Applications:
Especially useful for identifying fungal organisms, such as Aspergillus, Candida, and Cryptococcus, as well as certain bacteria in infected tissues.
Periodic Acid-Schiff (PAS) Stain
The PAS stain highlights carbohydrate-rich components, making it useful for identifying fungal organisms and detecting certain polysaccharide-containing structures in bacteria and parasites.
Principle:
Periodic acid oxidizes polysaccharides in microbial cell walls to aldehydes, which then react with Schiff reagent, producing a magenta color.
Materials:
- Periodic acid
- Schiff reagent
- Hematoxylin (counterstain)
Procedure:
- Deparaffinize and hydrate tissue sections.
- Treat with periodic acid for 5-10 minutes to oxidize carbohydrates.
- Rinse with water.
- Apply Schiff reagent for 15-30 minutes, reacting with aldehydes to form a magenta color.
- Rinse in tap water until color stabilizes (5-10 minutes).
- Counterstain with hematoxylin for 1 minute.
- Rinse, dehydrate, and mount. Fungal and carbohydrate structures will appear magenta against a blue background.
Interpretation:
Fungal elements, such as yeast and hyphae, and certain parasitic cysts appear magenta or pinkish-red against a light background.
Applications:
Primarily used for identifying fungi in tissue samples but can also highlight encapsulated bacteria like Klebsiella and structures in parasitic cysts.
Immunohistochemical (IHC) Staining
IHC staining uses specific antibodies to detect microbial antigens, allowing precise identification of particular pathogens.
Principle:
Antibodies bind to specific antigens present on microorganisms, and a secondary antibody conjugated to an enzyme (such as horseradish peroxidase) or fluorescent tag is used to visualize the complex.
Materials:
- Primary antibody specific to the target microorganism
- Secondary antibody conjugated to an enzyme (e.g., horseradish peroxidase)
- Chromogen (e.g., DAB)
- Blocking solution
Procedure:
- Deparaffinize and hydrate tissue sections.
- Block non-specific binding with a blocking solution (e.g., BSA) for 10-15 minutes.
- Apply the primary antibody and incubate (often for 30-60 minutes at room temperature).
- Rinse with PBS.
- Apply the enzyme-conjugated secondary antibody and incubate.
- Rinse with PBS.
- Apply the chromogen (DAB), allowing the color to develop for 5-10 minutes.
- Rinse with water, counterstain (if desired), and mount. Targeted antigens will appear as a brown stain.
Interpretation:
Targeted microorganisms are visible as brown (DAB substrate) or other colorations against the background.
Applications:
Effective for detecting viruses (e.g., cytomegalovirus, herpesvirus), bacteria, fungi, and protozoa. IHC staining is particularly valuable when other stains are inconclusive.
Fluorescent Staining (Auramine-Rhodamine and Direct Fluorescent Antibody Stains)
Fluorescent staining methods use fluorochrome-labeled dyes or antibodies to detect specific microorganisms.
- Auramine-Rhodamine Stain:
- Principle: Auramine-rhodamine binds to the lipid-rich cell wall of acid-fast bacteria, fluorescing under UV light.
- Procedure: Stain tissue sections with auramine-rhodamine dye, wash, and view under a fluorescence microscope.
- Interpretation: Acid-fast bacteria appear as bright yellow or orange under fluorescence.
- Applications: Primarily used for identifying Mycobacterium tuberculosis and other acid-fast organisms.
- Direct Fluorescent Antibody (DFA) Stain:
Principle:
Specific fluorescently labeled antibodies bind to microbial antigens.
Materials:
- Auramine-rhodamine stain
- Acid-alcohol (decolorizer)
- Potassium permanganate (counterstain)
Procedure:
- Fix the tissue section on a slide.
- Apply auramine-rhodamine stain for 15-20 minutes.
- Rinse with water.
- Decolorize with acid-alcohol for 2-3 minutes.
- Rinse with water.
- Counterstain with potassium permanganate for 1 minute.
- Rinse, blot dry, and examine under a fluorescence microscope. Acid-fast bacteria will fluoresce yellow or orange against a dark background.
Interpretation:
Targeted microorganisms fluoresce brightly against a dark background.
Applications:
Used for identifying viruses like respiratory syncytial virus (RSV) and bacteria such as Bordetella pertussis and Treponema pallidum.
Warthin-Starry Stain
The Warthin-Starry stain is a silver variation that detects spiral bacteria like Helicobacter pylori.
Principle:
Like other silver stains, the Warthin-Starry method uses silver nitrate, which the bacteria reduce to form black deposits.
Procedure:
- Apply silver nitrate to the tissue section.
- Develop the stain to visualize the bacteria as black or dark brown structures.
Interpretation:
Spiral or rod-shaped bacteria, such as Helicobacter and Bartonella, appear dark against a light background.
Applications:
Especially useful for detecting Helicobacter pylori in gastric biopsies, contributing to diagnosing gastric ulcers and related conditions.
Giemsa Stain
The Giemsa stain is often used in microbiology and parasitology for detecting intracellular pathogens and certain blood parasites.
Principle:
Giemsa stain targets nucleic acids and certain cell components, rendering them blue or purple.
Materials:
- Giemsa stain solution
- Buffered water (pH 6.8-7.2)
Procedure:
- Deparaffinize and hydrate tissue sections.
- Stain with Giemsa solution diluted with buffered water for 20-30 minutes.
- Rinse with buffer and then water.
- Air-dry and examine under a microscope. Parasites and bacterial cells appear with dark purple or blue nuclei.
Interpretation:
Parasites like Plasmodium and Leishmania appear with dark purple or blue nuclei while surrounding cells are lighter stained.
Applications:
Commonly used to identify blood parasites (e.g., Plasmodium, Babesia) and intracellular bacteria like Chlamydia and Rickettsia.
Fite-Faraco Stain
The Fite-Faraco stain is a modification of the acid-fast stain that is gentler on tissue and used specifically for detecting organisms like Mycobacterium leprae.
Principle:
The stain prevents excessive decolorization, allowing for more delicate visualization of weakly acid-fast organisms.
Materials:
- Xylene-peanut oil mixture
- Carbol fuchsin stain
- Acid-alcohol (mild)
- Methylene blue (counterstain)
Procedure:
- Deparaffinize sections with a xylene-peanut oil mixture to preserve the waxy cell wall.
- Stain with carbol fuchsin for 15-30 minutes without heat.
- Rinse with water.
- Gently decolorize with a mild acid-alcohol solution.
- Rinse with water.
- Counterstain with methylene blue for 1 minute.
- Rinse, blot dry, and examine. Acid-fast organisms will appear pinkish-red against a blue background.
Interpretation:
Acid-fast bacteria, such as Mycobacterium leprae, appear pinkish-red against a pale background.
Applications:
Used primarily in detecting Mycobacterium leprae in biopsies, aiding in diagnosing leprosy.